Abstract
High blood pressure is the leading cause of death and morbidity globally. The disease poses more health risks to people with underlying chronic conditions. Most patients with hypertension have not conceptualized its severity, and they expect it to be curable, therefore, failing to follow self-management practices. Apart from physical exercise and dietary observations, several antihypertensive agents have been proven effective. The main pharmacological drug classifications discussed include diuretics, alpha-blockers, beta-blockers, angiotensin-converting enzyme inhibitors, and calcium channel blockers. They reduce systemic vascular resistance, cardiac output, and blood volume. Research on hypertension’s pathophysiology revealed that renal malfunctions, microcirculatory changes, neural mechanisms, and environmental factors are attributable to high blood pressure development. Therefore, the advanced nursing practice should focus on patient education and personalized treatment interventions to improve health outcomes among patients living with hypertension.
Introduction
The heart pumps blood to all parts of the body through the blood vessels. Hypertension or high blood pressure refers to the persistent increase in blood pressure in the blood vessels. If the pressure is significantly high, the heart strains to pump blood, and it eventually fails. This condition is the leading cause of morbidity and mortality globally. It increases the risk of all major cardiovascular problems, such as stroke, abdominal aortic aneurysm, heart failure, sudden cardiac arrest, peripheral vascular illness, and coronary heart disease (World Health Organization, 2017). The study of hypertension’s pathophysiology clarifies the complex causes of the illness. Taddei et al. (2018) state that high blood pressure originates from the dysregulation of various homeostatic systems influencing the normal blood pressure and progressing organ damage, leading to hypertension. Most researchers claim that the disease follows complex interactions between the environment genetic factors, which result in various risks and hastens its period of onset among populations. This report analyzes hypertension’s pathophysiology, pharmacological agents used to treat it, and important information related to advanced nursing practice.
Pathophysiology of Hypertension
The body maintains normal blood pressure by balancing peripheral vascular resistance and cardiac output. Taddei et al. (2018) found that individuals with arterial blood pressure are more likely to have elevated cardiac output, leading to systemic vascular resistance. This idea guides physicians to understand the end physiological changes raising blood pressure. However, many neural, endocrine, renal, and cardiovascular control systems influence vascular and cardiac homeostasis, increasing the complexity of hypertension’s pathophysiology (World Health Organization, 2017). These factors differ among populations because gene-environment relationships modify them. Therefore, high blood pressure’s pathophysiology can be understood clearly by reviewing the role of its regulatory systems.
The renal system plays an important role in hypertension pathophysiology because the kidney regulates blood pressure. It specifically regulates the relationship between pressure-natriuresis and how the renin-angiotensin system works (Taddei et al., 2018). Moreover, damaged renal blood flow induces the perturbation of renal physiology (World Health Organization, 2017). Uncontained damage, apart from raised oxidative stress patterns and nephritic swelling, leads to high blood pressure. Variation in salt intake also influences the body’s blood pressure. Chisolm (2017) asserts that hypertension may arise from the kidney’s failure to excrete salt effectively. Therefore, the kidney must excrete sodium to balance such processes as high peripheral vascular resistance, which elevates blood pressure.
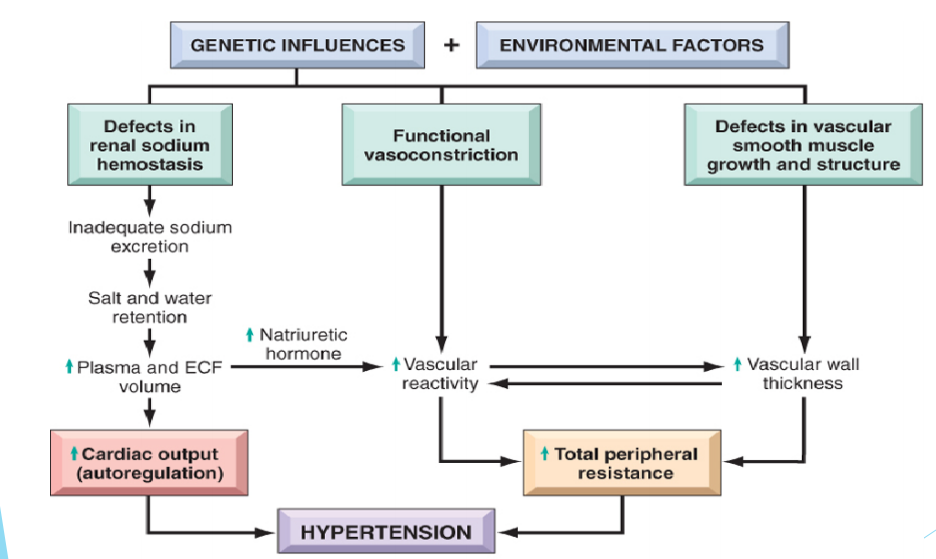
Apart from renal factors, microcirculatory changes, neural mechanisms, and environmental factors are attributed to hypertension development, primarily in the systo-diastolic and diastolic forms. These two conditions arise from peripheral resistance increase and volume overload. Arterioles and small arteries control peripheral resistance (Taddei et al., 2018). Thus, arteriolar reduction in density and changes in small arteries increases the risk of developing blood pressure. Neural mechanisms also play a crucial role in the pathophysiology of hypertension because they control cardiovascular homeostasis. Sympathetic stimulation induces blood pressure through various mechanisms, including cardiac contraction, decreased nervous capacitance, the variation of water and sodium release, and peripheral vasoconstriction (Klabunde, 2017). Environmental factors, Taddei et al. (2018) states that populations living in non-industrialized regions are less vulnerable to high blood pressure and age-related cardiovascular problems. Familial history is recognized in environmental causes, such that a family member with hypertension is likely to have offspring with high blood pressure. The schematic diagram in Figure 1 summarizes the pathophysiology of hypertension.
Pharmacological Agents Used to Treat Hypertension
Medics use various pharmacological agents to treat high blood pressure by reducing blood volume, systemic vascular resistance, and cardiac output. Klabunde (2017) and the World Health Organization (2017) classify antihypertensive drugs as follows “calcium channel blockers, angiotensin converting enzyme inhibitors, diuretics, alpha-blockers, angiotensin II receptor blockers, and beta-blockers” (p.6). Beta-blockers and calcium channel blockers form cardio-inhibitory drugs (Taddei et al., 2018). Some of these medications are combined depending on the status to increase their effectiveness.
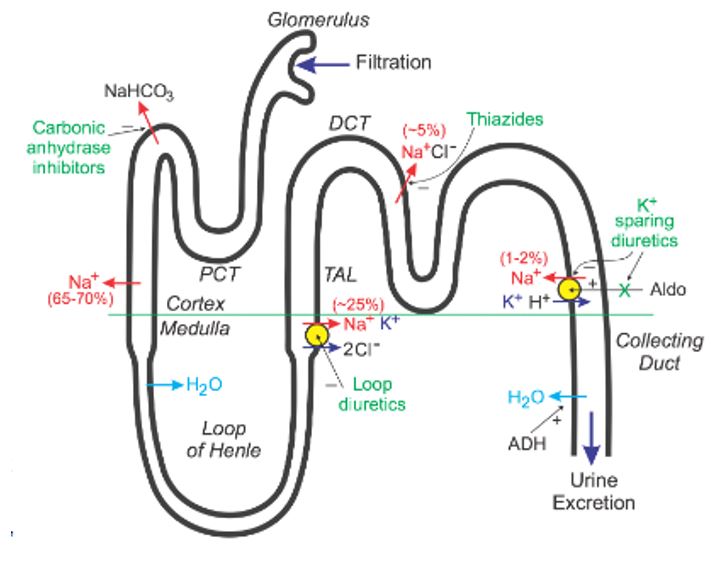
Diuretics are further classified into loop diuretics, thiazide diuretics, and potassium-sparing diuretics. These drugs mainly promote diuresis; increase in urine output by influencing how the kidneys manage sodium (World Health Organization, 2017). They inhibit sodium reabsorption at different regions of the tubular system. Many a time, doctors combine two diuretics to increase synergistic effect because one nephron can resolve affected sodium intake at another nephron. Hence, having many blocked nephron sites increases diuretic efficacy. Figure 2 below shows the action path of diuretic drugs.
Most antihypertension drugs mainly act on systemic vascular resistance, while some of them trigger vasodilation as they interfere with the sympathetic adrenergic vascular tone. They can also induce vasodilation by preventing the formation of angiotensin II and its vascular receptors (Chisolm 2017). Similarly, some of these drugs cause direct and mixed arterial dilation (Taddei et al., 2018). Beta-blockers primarily inhibit contractility and depresses heart rate by blocking the effects of sympathetic nerves on the heart. On the other hand, non-dihydropyridines calcium channel blockers reduce cardiac output by reducing heart rate and contractility. Others, including dihydropyridines, reduce systemic vascular resistance.
Further, cardio-inhibitory medications cause chronotropy, which is the decrease in heart rate, depress cardiac performance. They also cause myocardial contractility, which refers to a decrease in cardiac output and pressure in arteries. Klabunde (2017) notes that cardio-inhibitory drugs depress the heart’s electrical conduction, apart from hindering its relaxation. As a result, myocardial oxygen intake and heart function become impaired. Despite such impacts, mechanical and metabolic effects of cardio-inhibitory suit treatment of hypertension and other cardiovascular complications (Klabunde, 2017). Another category includes vasodilation drugs, making the smooth muscle in the blood vessels relax, causing dilation (World Health Organization, 2017). This action leads to a fall in systemic vascular resistance and arterial blood pressure. The pharmacological mechanism of most vasodilation agents is suited to resistance vessels. For example, calcium channel blockers are vasodilators, and they inhibit cardiac electrical and mechanical action, apart from dilating blood vessels (Taddei et al., 2018). These effects enhance antihypertensive actions and trigger blockage of other therapeutic conditions, for example, arrhythmias.
Important Information Related to Advanced Nursing Practice
Antihypertension drugs have side effects, as other medications do, and the patient must understand them before consuming the drugs. The World Health Organization (2017) states that diuretics are likely to cause gout and electrolyte imbalance. Similarly, bradycardia and asthma are associated with beta-blockers, while alpha-blockers cause orthostatic hypotension. Calcium channel blockers cause edema, constipation, flushing, headache, and gingival swelling. On the other hand, angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors lead to angioedema, rashes, and dry cough. Although these problems are temporary and manageable, consumers should consult their doctors to address any unusual drug intake symptoms.
Apart from side effects, the advent of hypertension management methods has been outpaced by misconceptions. Jones et al. (2017) report that several potential barriers to an individual’s management of the disease are dominant among Africa Americans. Some of them have not conceptualized the severity of hypertension, expecting it to be curable. Moreover, lack of patient exposure reduces their chances of attempting weight loss, apart from neglecting dietary advice. Other factors, including behavioral norms, patient beliefs, and health literacy, hinder self-management and high blood pressure pharmacological treatment (World Health Organization, 2017). Therefore, nurses should be aware of the patient’s understanding of the disease to minimize knowledge deficits. Advanced nursing practice requires that caregivers prescribe medications and create personalized treatment plans to improve health outcomes.
Conclusion
Hypertension is among the major public health concerns that need urgent responses. There are increased awareness and treatment frameworks, but many people still develop the disease. This study presented the pathophysiology of hypertension, pharmacological agents used to treat it, and crucial insights for advanced clinical nursing practice. Some treatment agents include diuretics, beta-blockers, calcium channel blockers, alpha-blockers, angiotensin II receptor blockers, and beta-blockers. They present unique working mechanisms, and they can be combined to increase effectiveness. These drugs have substantial side effects, and the patient should be conversant with the kind of medication prescribed. They should not stop using the drugs once blood pressure drops unless advised by a physician. The research demonstrated that most patients’ approach to self and advanced management is affected by health literacy, behavioral norms, and personal beliefs. Advanced nursing practices should focus on understanding a client’s knowledge of the disease for effective management.
References
Chisolm, O. E. (2017). Pathophysiology of hypertension and hypertension management. Web.
Jones, L. M., Rosemberg, M. A. S., & Wright, K. D. (2017). Opportunities for the advanced practice nurse to enhance hypertension knowledge and self-management among African American women. Clinical Nurse Specialist CNS, 31(6), 311-318. Web.
Klabunde, R. E. (2017). Cardiovascular pharmacology concepts. Cvphermacology. Web.
Taddei, S., Bruno, R. M., Masi, S., & Solini, A. (2018). Epidemiology and pathophysiology of hypertension. In A. J. Camm, T. F. Lüscher, G. Maurer & P. W. Serruys (Eds.), ESC CardioMed (3rd ed., pp. 2377-2388). Oxford University Press.
World Health Organization. (2017). Medication and management of associated diseases for patients with hypertension. Web.
