Introduction
The COVID-19 lockdown has lasted for more than a year already in many nations around the world. The stated cause behind the decision to extend it to that degree is that it is still not safe for people to operate as they had before the pandemic. Several different vaccines have been deployed to help protect people from the virus, but it is not feasible to vaccinate everyone, both in terms of the time required to do so and due to matters such as personal consent. However, the same considerations apply to many other virulent diseases, including poliomyelitis and the flu. While these illnesses may be more dangerous than COVID-19 once one becomes infected, poliomyelitis has nearly been eradicated around the globe, and the flu is manageable without lockdowns. A large part of the reason for humanity’s success in controlling these illnesses is a concept known as herd immunity.
As the name implies, herd immunity is a state in which a community as a whole is not threatened by an infection. For the disease to endure and propagate, it needs its current carriers to spread it to one or more people before they either die or return to a healthy state. However, people who have already had the illness or been vaccinated can no longer be infected. Hence, the ability of the carrier to infect others falls, and when they are only able to spread the infection to one person or fewer, the disease will eventually die out due to a lack of hosts. The specific proportion of the population that needs to be immune for this to succeed varies based on the particular infection’s ability to spread, but Fontanet and Cauchemez (2020) claim that it is at least 50% in the case of COVID-19. Concerns such as the longevity of the developed immunity notwithstanding, lifting the lockdowns should be strongly considered once this figure is achieved.
The researcher will collect data among their fellow students, who live in various communities and therefore represent a variety of situations. The directory of students will be requested from the administration and used to select individuals for sampling purposes. They will use simple random sampling to contact 200 people and ask them whether they have had COVID-19, tested positive on an antibody test (in the case of the asymptomatic variety), or been vaccinated. The survey will consist of a few simple demographic questions and a question regarding the presence of probable cause to expect the individual to be immune. All of the questions will be multiple-choice, with demographic data divided into several separate categories and the immunity question presenting a number of variants for the person to answer. The level of significance that the researcher will aim to achieve is 95%.
Data Collection Issues
Overall, the data collection proceeded according to plan, with the researcher successfully contacting students and receiving a response from most of them. No changes to the procedure needed to be made, and the data collection was successful. With that said, the researcher received a number of responses where the participants expressed a desire to mark several of the choices. Most often, this happened when people had COVID-19 or suspected that they did and got tested afterward. As a result, they wanted to mark both options in the survey or were unsure which one to choose. The researcher recommended these people to mark the test-related response, as its confirmation of the antibodies’ presence supersedes the suspicion thereof that results from one overcoming the condition. Possibly in part as a result of this approach, they received surprisingly few “I have had COVID-19” responses.
Hypothesis Test Results
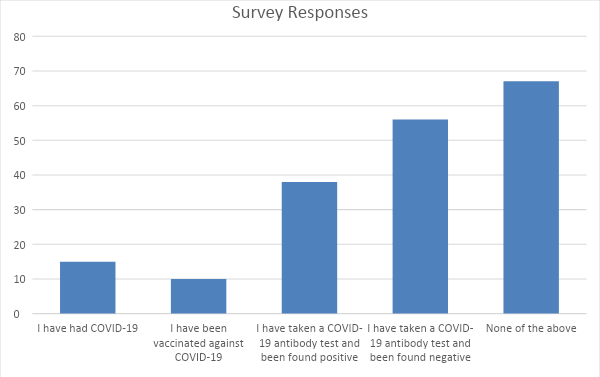
Ultimately, the researcher received admissible responses from 186 people, 63 of whom reported an answer that indicated the likely presence of COVID-19 immunity. This number represents a 33.9% proportion of the sample, which can be derived from Fig. 1, which is considerably lower than the expected 50% figure. The null hypothesis, in this case, is that the proportion of the people who have developed immunity to the disease is lower or equal to 50%. The alternative hypothesis is that the percentage is higher than 50%. Assuming a normal distribution with a mean of 50%, the researcher found that the z-score of the observed statistic was -4.65. To qualify for the rejection of the null hypothesis, it would have to be 1.96 or more, given the 95% confidence level. As such, the null hypothesis is accepted, and the alternative hypothesis is rejected.
Results Summary
With the null hypothesis accepted and the alternative hypothesis rejected, the conclusion is that less than 50% of the population has developed immunity to COVID-19. With that said, the research was influenced by several biases, most notably selection bias. By choosing only their fellow students as sample participants, the researcher has limited the choice to a very specific demographic, limited in terms of age and socioeconomic status as well as several other variables. Another potential bias is data collection bias, as the researcher relied on self-reported immunity results. Nearly a third of the respondents answered “None of the above,” which was assumed to mean “no immunity.” In reality, a variety of options is possible, such as the respondents having an asymptomatic case of COVID-19 and developing immunity without realizing it. Overall, while the results were initially unexpected, in hindsight, they appear to be reasonable given the number of reported COVID-19 cases nationwide relative to the total population. The research could be expanded to involve more people and testing rather than self-reporting, but the researcher expects that it would yield similar results.
Conclusion
The researcher was testing the claim that the U.S. population has developed herd immunity to COVID-19, defined as at least 50% of it has developed antibodies. This assertion was tested with a significance level of 95%, which is standard and reliably accurate. To gather data, the researcher contacted a sample of 200 students and received responses from 18 of them. They asked the question of whether the respondent has had COVID-19, been vaccinated, or undergone testing (as well as what result it returned). The hypothesis test rejected the claim, as it found only 33.9% of the sample to have their immunity reasonably confirmed. With that said, the situation may change as efforts to vaccinate the population progress, and additional research elaborates on the longevity of COVID-19 antibodies. As such, a study with a larger population that relies on testing for each participant may be warranted in the future.
Reference
Fontanet, A., & Cauchemez, S. (2020). COVID-19 herd immunity: Where are we? Nature Reviews Immunology, 20(10), 583-584.
