Introduction
Pulmonary disease in the geriatric period is the most dangerous illness, as it affects all vital systems and can significantly complicate the course of the underlying disease. Medical care should always be qualified, but in this case, more attention should be paid to individual characteristics. Patient-centered nursing theory is appropriate for this because it addresses four key components of treatment at once: culture, care, communication, and collaboration (Santana et al., 2018). The traditional nursing approach is the central compulsory part of treatment, but nurses try to solve patients’ problems with medicine and try to find the best solution to meet disturbing needs (Kuipres et al., 2019). With this approach, it is possible to change perceptions of care and solve problems faster and better.
The Patient-Centered Approach
The patient-centered approach to nursing was developed by Faye Abdellah at the beginning of World War II for better nursing management and education. Nowadays, this theory is relevant and necessary in view of the transition to patient-centered practice and regular professional development. This approach allows nurses to critically assess the situation and analyze the patient’s needs: whether the shortness of breath is really caused by COPD and not a criterion for VAP (Ospina et al., 2018). In addition, the approach offers new ways of making clinical decisions: the choice of bronchodilators and mucolytic, the need to take theophylline, and the search for oxidative stress factors. This theory combines the principles of participation and collaboration, as well as the full exchange of objective information (Hashim, 2017). Nurses build a trusting relationship with patients, and they are more easily contacted, which increases the effectiveness of treatment and care.
Nursing Care Plan for COPD with Suspected VAP
Developing a nursing care plan for the case in question requires setting an expected goal by the impaired needs. To do this, the nurse performs a nursing examination and determines the patient’s characteristics: ethnicity, age, smoking history, and chronic diseases. The patient is Native American and is 75 years old, and continues to smoke, aggravating COPD. His condition can be characterized as severe, so the nurse should think carefully about the plan of care. In addition, the nurse draws attention to the peculiarity of the course of the postoperative period: breathing difficulties persist and probably a low saturation of less than 90%. In this regard, a goal and expected result can be set: the saturation level in the next five days of treatment will reach 90%, and the condition will become average. The goal will be relief of breathing and stabilization of the general situation.
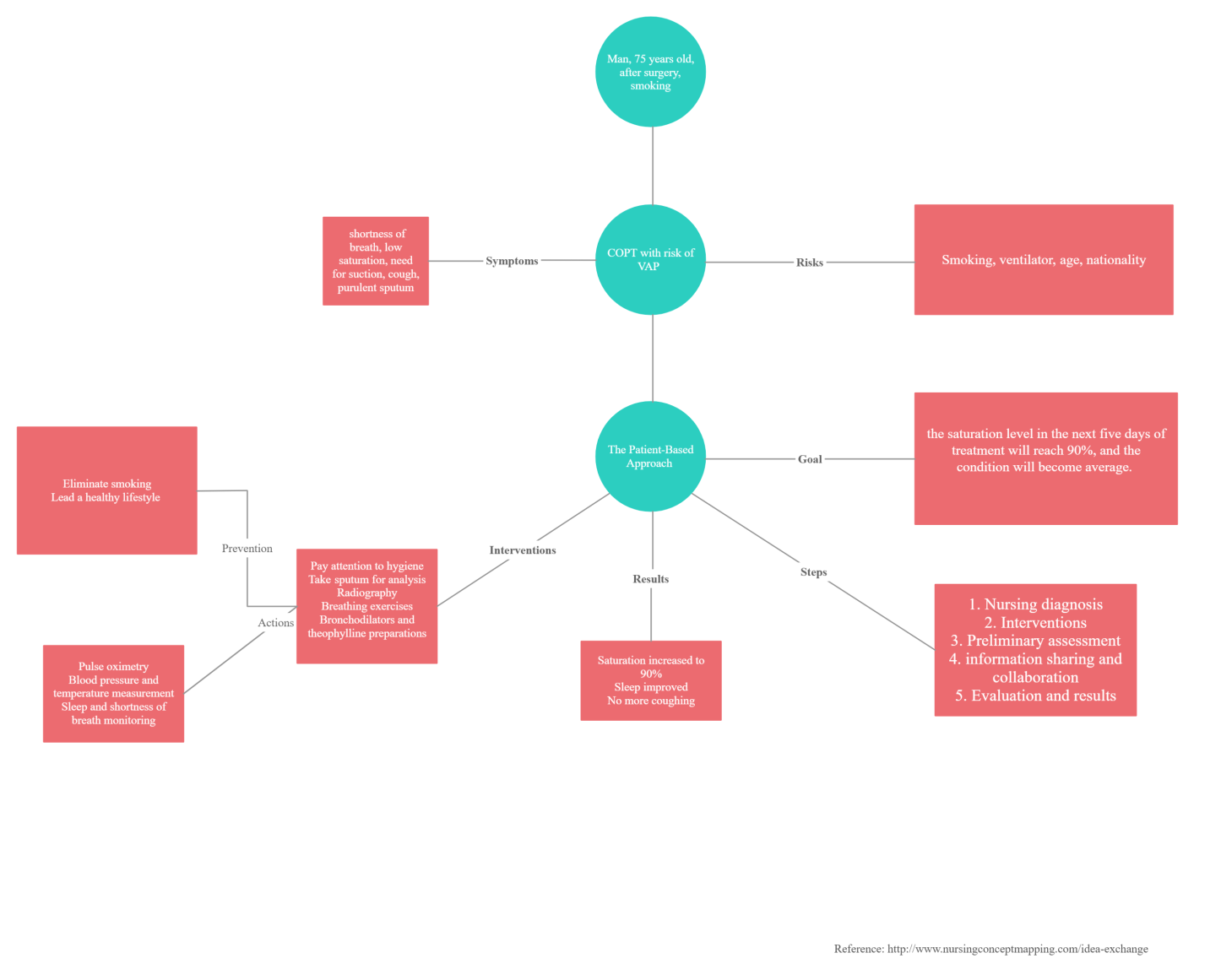
A nursing care plan based on patient-centered theory consists of ten items, but it would be appropriate to adjust it to five steps. The plan was visualized and presented in a concept map reflecting the main features (see Appendix).
1. Making a nursing diagnosis after examination: choking attacks, cough, elevated BP, and risk of infection. This diagnosis is justified by objective data: prolonged stay on the ventilator, the need for frequent suctioning of fluids, the general severity of the postoperative period (Ospina et al., 2018). The data allow the nurse to assess the situation and think about future interventions. The diagnosis will be used to create medication and a physiological treatment plan.
2. Interventions are determined according to impaired needs, mainly breathing difficulties. In addition, the staff suggests the risk of developing an infection, VAP, so the nurse should pay extra attention to hygiene (Kuipres et al., 2019). The patient has a cough, so nurse should take sputum for microbiological and general analysis. The nurse should perform regular pulse oximetry to monitor saturation and pressure levels. It will be advisable to refer the patient for an X-ray to clarify the degree of pulmonary obstruction (Ospina et al., 2018). A severe condition requires breathing exercises and physiologic activity to avoid bedsores and complications. Hyperdynamic can also affect hemostasis, so the nurse should monitor the intake of bronchodilators and theophylline preparations. It is worth paying attention to smoking prevention, as it makes treatment much more difficult.
3. After the first interventions, the nurse assesses the condition: the patient will breathe more accessible, the respiratory rate will stabilize. Sleep problems are likely to disappear, coughing will become rare, and sputum will be clear. The main goal is to achieve average saturation values, and the nurse can use pulse oximetry’s charts(Ospina et al., 2018). It is also essential to pay attention to the social aspect during the evaluation phase. If possible, the nurse should communicate with the patient and build rapport to convince them to stop smoking. Interaction with the family can also help build relationships and improve prevention.
4. This stage is devoted to information exchange and consultation with other nurses. Exchanging information with the patient and relatives will allow the nurse to convey objective data and explain the need for compliance with all recommendations (Hashim, 2017). Establishing contact with the patient is the goal of the theory used, and it should not be neglected. Sharing information with other nurses will provide a critical perspective from a different angle (Santana et al., 2018). For example, additional recommendations will improve hygiene and help adjust preventive care.
5. In the final phase, the last interventions of the developed plan are conducted, and the final results are evaluated. It is expected that saturation will increase to 90%, and the patient will not need ventilator ventilation. The respiratory rate will be reduced to fair values at which there will be no significant strain on the body. At this stage, the nurse communicates with the patient and tries to agree. The focus is on continuing treatment to avoid complications (VAP) and the transition to a healthy lifestyle.
Conclusion
Thus, the developed plan meets the requirement of the patient-centered theory of nursing approach. The program includes five steps, each of which the nurse focuses on culture, care, communication, and collaboration. The nurse diagnoses and defines a goal for which saturation-enhancing interventions are conducted. Based on the plan, the patient is expected to feel relief, and breathing problems become less pronounced.
References
Hashim, M. J. (2017). Patient-centered communication: Basic skills. American Family Physician, 95(1), 29-34.
Kuipres, S. J., Cramm, J. M. & Nieboer, A. P. (2019). The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Services Research, 19(13). Web.
Ospina, M. B., Michas, M., Deuchar, L., Leigh, R., Bhutani, M., Rowe, B. H., Marciniuk, D., Goodbridge, D., Dechamna, G., Bourbeau, J., Balter, M., Camp, P., Hernandez, P., Goldstein, R. S. & Stickland, M. K. (2018). Development of a patient-centred, evidence-based and consensus-based discharge care bundle for patients with acute exacerbation of chronic obstructive pulmonary disease. BMJ Open Respiratory Research, 5, 1-9. Web.
Santana, M. J., Manalili, K., Jolley, R. J., Zelinsky, S. Quan, H. & Lu, M. (2018). How to practice person‐centred care: A conceptual framework. Health Expectations, 21(2), 429-440. Web.
Appendix
Concept Map of Nursing Care Plan