Exocrine gland dysfunction is the most common symptom of cystic fibrosis, a genetic illness caused by a mutation in a specific gene. A duct or aperture on the body’s surface is where exocrine glands secrete bodily secretions such as sweat, tears, saliva, milk, and digestive juices. Sweat, lacrimal, salivary, mammary, and digestive glands are among the unusual glands. The infection of cystic fibrosis to the exocrine glands causes the thickening abnormality of the secretions, which causes clogging, leading to inflammation, obstruction and infection. Furthermore, fibrosis can cause multiple endocrine disorders, including short stature, bone disease, and diabetes (Barry, 2021). This paper aims to research cystic fibrosis, the central body parts, normal physiology of the body system affected, mechanism of the pathophysiology, prevention, and treatment.
Anatomy of the Body System Affected by Cystic Fibrosis
The central body organs affected are the lungs, pancreas, and the intestines, in which, upon infection, mucus and clogs are produced. The infection might lead to certain disorders in the body, including; malnutrition, poor growth, frequent respiratory infections, chronic lung disease, and breathing problems. The study of the functioning of the major parts affected by the the cystic fibrosis is quite essential in understanding it effects.
Anatomy of Normal Lungs
The lungs from the major organs of the body of the respiratory system, whose function is to oxygenate the blood. The lungs are divided into two major sections; the right lungs and the left lungs. The right lungs with three labels are slightly larger than the left lung with two labels.
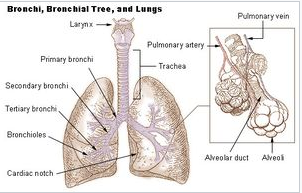
The mediastinum, which houses the heart, trachea, esophagus, and lymph nodes, separates the lungs (Morrison, 2019). The diaphragm’s abdominal cavity is divided from the heart’s chest compartment by a membrane known as the pleura. The lung root separates the left and right lungs from the mediastinum, forming structures entering and exiting the lungs. Several mediastinal structures are adjacent to the left and right lungs: the heart, arch of the aorta, the thoracic aorta, and the esophagus are all close to the left lung, while the azygous vein is near the right lung.
Anatomy of a Normal Pancreas
Sugar, carbohydrates, and lipids are broken down by the elongated, tapering pancreas positioned across the lower abdomen from the stomach, where it secretes pancreatic juice. It also manufactures the hormones insulin, glucagon and gastrin. The right side of the pancreas is the widest; hence it is referred to as the head. The pancreas directly links the stomach, duodenum, transverse mesocolon, common bile duct, and spleen organs in the abdomen. Furthermore, the pancreas is positioned ear several major vessels, namely, the aorta and the inferior vena cava. This superior mesenteric artery lies behind the neck of the pancreas, the posterior mesenteric artery to the neck, the splenic artery
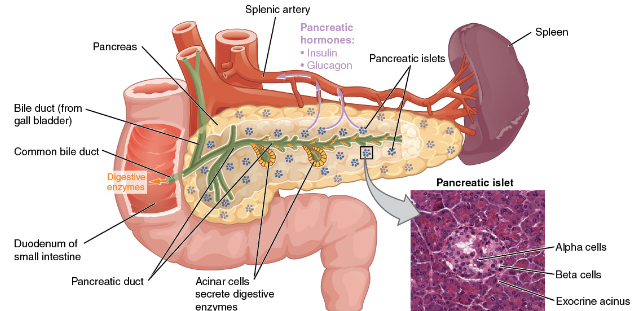
The pancreas is a retroperitoneal organ made up of five parts and an external system of ducts. Pancreatic arteries supply the pancreas. The arteries originate from neighboring vessels stated above. Furthermore, it is innervated by the vagus nerves, celiac plexus, and superior mesenteric plexus.
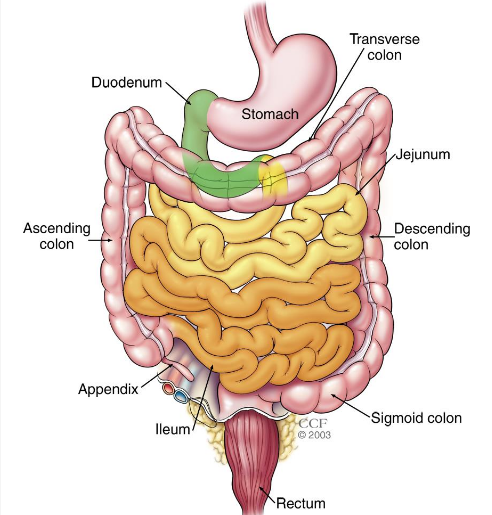
Anatomy of a Normal Intestine
There are two sets of intestines: the small and large intestines. The gut may absorb nutrients and water. The rectum and the small intestine make up the intestines. About 20 feet in length and an inch in diameter, the 3instine is the smallest of the three. The duodenum, jejunum, and ileum are the three sections of the small intestine. There are around 5 feet of the large intestine in the human body. The digestive system includes the small intestine. This is why the small intestine is called the small intestine; its lumen is smaller. When food is swallowed, it goes via the small intestine, breaking it down and absorbing it. The duodenum, which links the small intestine to the stomach, is located on the small intestine’s proximal end. The ileum, which connects the small intestines to the large intestine, is located at the end. It is located between the duodenum and the intestines, the jejunum. Approximately 10 to 15 inches in length, the duodenum is the smallest part of the digestive tract. It is located in the small intestine and serves as a marker by marking where the bile duct and pancreatic duct discharge their digestive juices into the small intestine,
Normal Physiology of the Body Parts Infected by Cystic Fibrosis
Normal physiology involves the study of the normal functioning of the body organs.
Physiology of the Lung
The lungs from the fundamental of the body organs whose essential function is to facilitate the exchange of air from the environment to the bloodstream. The oxygen inhaled travels the alveoli into the capillary networks, where it can enter the arterial systems. The lungs’ basic activities include inhaling and exhaling gasses, exchanging gases between the lungs and the circulatory organs, exchanging internal respiration, exchanging gases between the blood system and bodily tissue, and olfaction. The respiratory system is composed of the nose, larynx, trachea, bronchi, bronchioles and lungs.
Physiology of the Pancreas
The pancreas functions as a digestive and hormonal function. During the digestive process, it generates enzymes that assist in breaking down carbohydrates in the gastrointestinal tract, undigested lipids from the stomach, proteins, and acids in the duodenum and other substances. Enzymes secreted by the pancreas go from the pancreas to the duodenum, where they are activated. Furthermore, the other primary pancreatic function is the production of the hormone, which helps regulate blood sugar level and appetite, aids in the stomach acid stimulation, and tells the stomach when to empty.
Physiology of the Intestines
The intestines, which form the digestive system, function to break down food. The small intestine forms part of the gastrointestinal tract that follows the stomach and functions to digest food, absorb nutrients from ingested food. Moreover, the large intestine is responsible for processing indigested food materials. The large intestine comprises four main parts: the cecum, ascending colon, transverse colon, descending colon, and sigmoid colon.
Mechanism for Pathophysiology
The CF transmembrane conductance regulator (CFTR) gene has a mutation that causes cystic fibrosis. The CFTR protein, which is produced by the cystic fibrosis gene, controls the flow of chloride and sodium ions across the membrane of epithelial cells. When cystic fibrosis is activated in the body, it causes some pathophysiological impact by causing severe damage to the body organs. The mechanism of the pathophysiology of the pathogen include:
The Mechanism for Pathophysiology in the Lungs
Cystic fibrosis disease patients often experience failure of innate airway defense mechanisms in the lungs. In the initiation of cystic fibrosis in the lung, symptoms such as mucus dehydration is exhibited by the infected. The pathogen then causes the thickening of the mucus in the lungs. The thickened mucus blocks the airway leading to heart damage hence disabling the functions of the lungs.
Mechanism of Pathophysiology in the Pancreas
Cystic fibrosis infection in the pancreas causes its inefficiency. The pathogen causes ductal plugging in the pancreas as it leads to the secretion of deficient fluid secretion in the pancreas, leading to pancreatic protein hypersecretion. Therefore, the tubes responsible for the secretion of digestive food and hormones are blocked with mucus. The blocking of the small tubes leads to the cumulation of the enzymes and the hormones in the pancreas hence its inflammation.
The Mechanism for Pathophysiology in the Intestines
The infection of cystic fibrosis in the intestines leads to the deficient union in fluid transport in the intestines due to thickening, leading to the alteration of the luminal environments, hence causing CF to impair the turnover and clearance of mucus. The disorder also led to abnormal colonization, which is caused by static mucus. The sticky mucus in the digestive tract blocks the pores to absorb digested food, nutrients and fats into the body.
Prevention
An inherited gene causes cystic fibrosis; hence it cannot be prevented. Its mutative nature makes its cause challenging to evaluate, as it stays dormant up to a given age when it starts attacking the patient’s organs. Most fibrosis start showing at the age of 6-8 months, while some other patients are diagnosed at 1year (Marquez Loza, 2019). CF’s rate of infection highly depends on the rate of disease progression in the organs. Therefore, once one is diagnosed with CF, no medical procedure can prevent it.
Treatment
When one is diagnosed with the cystic fibrosis gene, the patient is taken through an intense procedure to prevent it from causing the malfunctioning of vital body organs. For chest infections such as mucus cumulation in the lungs, the patient is given antibiotics to prevent CF from causing further damage to the patient (Marquez Loza, 2019). The antibiotics also make the mucus thicker and easier to cough up. Antibiotics also broaden the airway and reduce inflammation.
References
Atkinson, M. A., Campbell-Thompson, M., Kusmartseva, I., & Kaestner, &. K. (2020). Organisation of the human pancreas in health and in diabetes. Diabetologia, 63(10), 1966-1973. Web.
Barry, P. J.-D. (2021). Triple therapy for cystic fibrosis Phe508del–Gating and–residual function genotypes. New England Journal of Medicine,, 385(9), 815-825. Web.
J.KastlJr, A., A.Terry, N., DWu, G., & G.Albenberg, &. L. (2020). The Structure and Function of the Human Small Intestinal Microbiota: Current Understanding and Future Directions. Cellular and Molecular Gastroenterology and Hepatology, 9(1), 33-45. Web.
Kahathuduwa, C. Respiratory Physiology – Introduction. Web.
Marquez Loza, L. I. (2019). Lentiviral vectors for the treatment and prevention of cystic fibrosis lung disease. Genes, 10(3), 218. Web.
Morrison, C. B. (2019). Mucus, mucins, and cystic fibrosis. Pediatric pulmonology, 54, S84-S96. Web.
