Introduction
PICOT: In women at high risk of developing breast cancer (P), how does an ARNP-conducted consultation (I) affect their willingness to use mammography (O) right after the consultation and ten weeks after it (T) as compared to the willingness to use mammography before the consultation (C)?
Methodology and Research Design
The study is going to take the form of a pre-test post-test qualitative research. There will be one group of participants, in which the effects of the intervention will be measured by checking the women’s attitudes towards mammography before and after the ARNP-led consultation. The study will use a tool that generates ordinal (quantitative) data, which will be analyzed quantitively. The chosen methods are appropriate for the aim of the study, which is to determine the effectiveness of the intervention.
Setting/Sample Design
The study will take place within preventive and primary care settings (a community clinic). The sample will consist of ARNPs and women with high risks of developing cancer who should be recommended the use of mammography. The only exclusion criterion is belonging to vulnerable populations. Currently, senior women (older than 60 years) are not supposed to be recruited, but it is acknowledged that age is one of the factors that are associated with the need to use mammography (Nattinger & Mitchell, 2016). Consequently, the exclusion criteria may be adjusted to include older women who can consent to participate (have no cognitive impairments).
It is planned to recruit between two and five ARNPs. Each of them will work with between 5 and 15 patients for a total of 25-35 patients. The ARNPs will identify eligible patients and inform them about the study. The women who are interested in participating will contact the researcher and receive extensive information about the study. Thus, the sampling method can be characterized as a mix of convenience and voluntary sampling with an element of quota sampling (Polit & Beck, 2017). The choice of the approaches is explained by the resources of the researchers and the importance of ensuring the consent of the participants (the nature of the discussed topic may be connected to negative feelings).
Confidentiality
No confidential or identifying information will be gathered throughout the study. The data collection tool (see Appendix A) focuses on the women’s perceptions regarding mammography. The collection procedures will use codes to distinguish the responses of the participants. No women or ARNPs will be identifiable from the final report because it will present consolidated results. The participants will be offered the details regarding confidentiality procedures in their informed consent forms.
Procedure/Intervention
The ARNPs will be required to determine the eligibility of potential participants, provide them with recruitment materials, receive and code the questionnaires, and conduct individually customized consultations on the use of mammography. The patients will be required to complete the questionnaire, attend the consultation with their ARNPs, complete the questionnaire immediately after the consultation, and then show up for a follow-up questionnaire ten weeks after the consultation. All the participants will be provided with informed consent forms before any activities.
Aligning Stakeholders
The key stakeholders of the study are the participants (both ARNPs and women), but it is also important to engage the management of the settings. The study will require little time from the patients, but the ARNPs’ contribution will be greater. Also, the study will take place directly in the settings. Consequently, the support of the management and ARNPs are crucial and will be ensured through negotiation and demonstration of the research that indicates the significance of the proposed study.
Instruments/Scales and Measurement of Outcomes
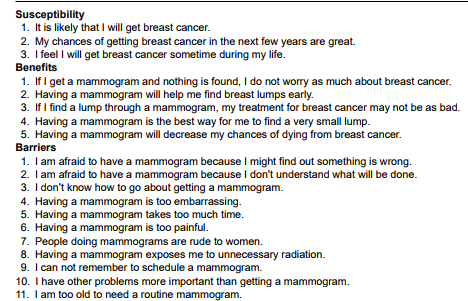
Champion’s (1999) Susceptibility, Benefits, and Barriers Scale for Mammography Screening (SBBSMS) is proposed as the data collection tool for the study (see Appendix A). SBBSMS remains valid for groups with various cultural backgrounds (Hasnain, Menon, Ferrans, & Szalacha, 2014; Wang, Hsu, Wang, Huang, & Hsu, 2014). Also, it helps to determine the perceived risks of developing cancer, the benefits of using mammography, and the barriers to it. Consequently, the tool can both guide the consultation and demonstrate its effectiveness in educating women and dispelling their doubts and incorrect assumptions.
Data Collection and Data Analysis
SBBSMS is based on a Likert scale (from “strongly agree” to “strongly disagree”), which means that it produces ordinal data. The data will be collected three times (before the consultation, immediately after it, and ten weeks after it). The results will be analyzed statistically to determine if significant changes can be traced. The type of analysis that appears to be appropriate for the task is Wilcoxon signed ranks test: it can be employed with ordinal data for pre-and post-test studies (Polit & Beck, 2017, p. 412). The results of the analysis will be gathered in the final report and presented to the researcher’s peers and instructors.
Significance of the Study
The study is significant because it addresses an understudied aspect of a topical issue: the effectiveness of ARNP-led interventions aimed at educating women about mammography. Indeed, preliminary research indicates that while consultations are expected to affect the use of mammography, no recent evidence directly considers their effectiveness (Donovan, Urquhart, Hopkins, Knight, & Moore, 2014; Gray et al., 2017; Haas et al., 2017; Percac-Lima et al., 2015). Similarly, few direct guidelines exist on ARNP-conducted consultations on the matter (Best, Spencer, Hall, Friedman, & Billings, 2014; Gray et al., 2017). Also, the importance of studying the methods of educating women is apparent (Percac-Lima, Ashburner, McCarthy, Piawah, & Atlas, 2015). Indeed, breast cancer is a major issue (Gagnon et al., 2016), and mammography can greatly reduce its negative consequences through timely diagnosing (Best et al., 2014). Consequently, the proposed study can contribute some evidence to this relevant discussion, which constitutes the significance of the research.
Assumptions and Limitations
It is expected that some of the limitations of the study can include the representativeness of the sample and self-reporting. The issues can be explained to an extent. Indeed, the primary inclusion criterion is the high risk of developing cancer, but this risk is higher for certain groups (Best et al., 2014). Consequently, it is assumed that such groups can become overrepresented in the study. This outcome is considered logical and is not viewed as a weakness of the study, although it is acknowledged that it may limit the applicability of the investigation. Given the nature of the data to be collected, it is also understandable that self-reporting should be employed: the intent to use mammography can only be checked through it. Regarding the selected sampling methods, they do not typically result in a representative sample (Polit & Beck, 2017), but their choice is explained by the needs and resources of the research. Thus, the limitations are the results of the specifics of the study and need to be considered.
Conclusions
The conclusions of the study will reflect its aim and be limited by the specifics of its design. The study will report the findings regarding the effectiveness of the intervention (ARNP-led consultation) in educating women on the use of mammography, which will be measured through SBBSMS and analyzed with the help of the Wilcoxon signed ranks test. Also, it will specifically focus on the limitations (sampling methods and the representativeness of the sample). The study will not be able to resolve the problem of the lack of research on the topic, but it will contribute some data to the discussion, which indicates its significance. This fact, along with the rigorous protection of participants’ confidentiality, will be employed to engage and align stakeholders.
References
Best, A., Spencer, M., Hall, I., Friedman, D., & Billings, D. (2014). Developing spiritually framed breast cancer screening messages in consultation with African American women. Health Communication, 30(3), 290-300. Web.
Champion, V. (1999). Revised susceptibility, benefits, and barriers scale for mammography screening. Research in Nursing & Health, 22(4), 341-348.
Donovan, D., Urquhart, L., Hopkins, U., Knight, S., & Moore, L. (2014). Oncology nursing support for safe and effective use of eribulin in metastatic breast cancer. Clinical Medicine Insights: Oncology, 8, 1-6. Web.
Gray, T., Cudjoe, J., Murphy, J., Thorpe, R., Wenzel, J., & Han, H. (2017). Disparities in cancer screening practices among minority and underrepresented populations. Seminars in Oncology Nursing, 33(2), 184-198. Web.
Haas, J. S., Barlow, W. E., Schapira, M. M., MacLean, C. D., Klabunde, C. N., Sprague, B. L.,… Harris, K. (2017). Primary care providers’ beliefs and recommendations and use of screening mammography by their patients. Journal of General Internal Medicine, 32(4), 449-457. Web.
Hasnain, M., Menon, U., Ferrans, C., & Szalacha, L. (2014). Breast cancer screening practices among first-generation immigrant Muslim women. Journal of Women’s Health, 23(7), 602-612. Web.
Nattinger, A., & Mitchell, J. (2016). Breast cancer screening and prevention. Annals of Internal Medicine, 164(11), ITC81. Web.
Percac-Lima, S., Ashburner, J., McCarthy, A., Piawah, S., & Atlas, S. (2015). Patient Navigation to improve follow-up of abnormal mammograms among disadvantaged women. Journal of Women’s Health, 24(2), 138-143. Web.
Polit, D.F., & Beck, C.T. (2017). Nursing research: Generating and assessing evidence for nursing practice (10th ed.). Philadelphia, PA: Lippincott, Williams & Wilkins.
Wang, W., Hsu, S., Wang, J., Huang, L., & Hsu, W. (2014). Survey of breast cancer mammography screening behaviors in Eastern Taiwan based on a health belief model. The Kaohsiung Journal of Medical Sciences, 30(8), 422-427. Web.
Appendix A
Data Collection Tool: The Questions of Champion’s (1999) Susceptibility, Benefits, and Barriers Scale for Mammography Screening
All the questions have Likert-scale answers from “strongly agree” to “strongly disagree.”