Introduction
The health of communities must be addressed in a well-planned manner considering the long-term effects of policies and barriers that obstruct their implementation. Leading Health Indicators (LHIs) are a subset of the Healthy People 2030 goals that were chosen to spur action for bettering health and wellbeing (“Health People 2030,” n.d.). The majority of LHIs focus on significant issues that have an impact on the leading causes of death and disease in the country. LHIs assist organizations, communities, and states all over the country in directing their resources and efforts toward enhancing everyone’s health and wellbeing.
Leading Health Indicator and Public Health Issue
Cigarette smoking is among the causes of several diseases such as cancer that substantially decrease the quality of life for individuals or lead to mortality. One of the LHIs of the Health People 2030 is to “reduce current cigarette smoking in adults — TU‑02” (U.S. Department of Health and Human Services, n.d., para. 1). According to the website’s data, 14.2% of adults are smokers, with the initiative’s target to reduce this number to 6.1% (U.S. Department of Health and Human Services, n.d., para. 1). Thus, the number of smokers should be reduced by more than 50% to address this goal of the Healthy People 2030.
System-level barriers to program implementation are the lack of policies that would actively ban cigarette smoking or make it more challenging for smokers to purchase cigarettes and use them. According to the American Lung Association (n.d.), “the country has made progress toward making all 50 states smokefree with 28 states1 and the District of Columbia having passed comprehensive smokefree laws” (para. 1). Thus, many states do not regulate the public use of tobacco, which subjects both the smokers and individuals exposed to the tobacco smoke to danger and health-related risks.
Moreover, the recent rise of e-cigarettes and vaping devices that contain nicotine is not addressed extensively by the existing regulations. American adults are more prone to consume cigarettes than any other tobacco product, and smoking causes cancer and early mortality (“Healthy People 2030,” n.d.). Price rises, media campaigns, and smoke-free laws are a few population-level strategies to reduce tobacco usage. However, today many people choose to smoke and become addicted to nicotine, and many use electronic cigarettes or tobacco-heating devices that are currently promoted by large companies. These devices and their health effect have not been studied extensively, and there is potential harm in the systemic use of these nicotine-containing products. Therefore, there is a systemic barrier that obstructs the government from rapidly addressing the health-related concerns of new devices and products that contain tobacco.
Smoking, especially in communities with high tuberculosis (T.B.) prevalence, is a significant factor in the premature death of T.B. patients (Zvolska et al., 2020). The most recent T.B. care guidelines emphasize the significance of including tobacco dependence treatment and smoking cessation in T.B. therapy. Raising the community’s awareness of the negative effects of smoking on T.B. patients’ health and adopting standardized TDT in accordance with guidelines within national T.B. programs may help this high-risk population quit smoking more frequently. Moreover, Zvolska et al. (2020) state that the negative attitudes toward smoking bans imposed by the government are one of the factors that serve as a systemic barrier to reducing the number of smokers in the U.S.
Education on the dangers of nicotine and ways of abandoning the addiction to nicotine is the systemic level policy that could help reduce the percentage of smoking adults. The government is already implementing policies that would restrict cigarette use and provide some information to the consumers about the dangers of this product; however, these efforts are not sufficient to help active smokers quit this habit. More attention should be dedicated to active campaigns that explain how people can quit smoking and what short-term and long-term effects they might experience if they choose to continue smoking. Cultural values and practices play a role in the success or failure of any intervention. Mainly, smoking tobacco is seen as a tradition in some cultures, and government policies would not affect these traditions significantly.
The interprofessional team that would work on intervention on tobacco use would consist of an addictions specialist, a general physician or a nurse practitioner, and a physiotherapist who can help patients overcome the phycological barriers that endure smoking. Since addiction is a complex problem that has underlying phycological, biological, and social elements, the cooperation of an interprofessional team is a necessity in this case. For example, the general physician can explain the biological changes that occur to a smoker’s body and the health-related risks that follow. The addiction specialist and therapist can help create strategies to quit smoking, such as ways of reducing the number of cigarettes or using cognitive-behavioral therapy to address the psychological drivers of smoking.
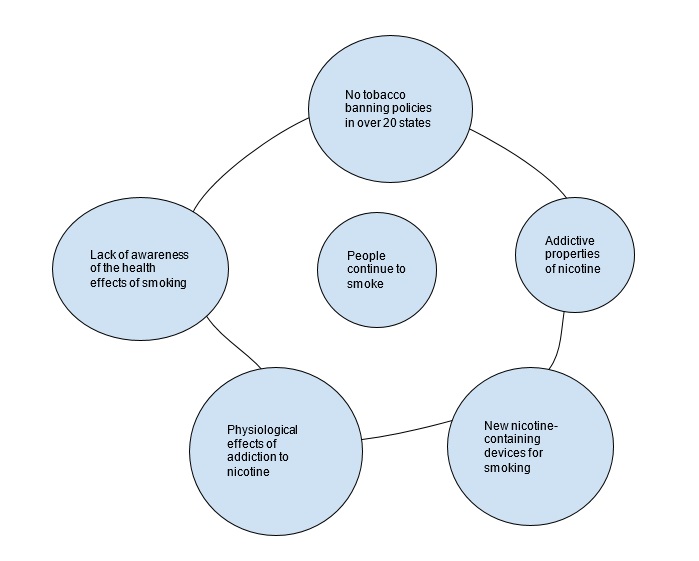
A Causal Loop Diagram presented in Figure 1 shows the complexity of relationships that impact the success of this intervention.
Conclusion
In summary, a portion of the Healthy People 2030 targets known as LHIs was selected to encourage action for improving health and wellbeing. The bulk of LHIs concentrate on important topics that have an effect on the most common illnesses and deaths in the U.S. Smoking plays a substantial role in the early demise of T.B. patients, particularly in areas where T.B. prevalence is high. The government is unable to effectively address the health issues raised by new tobacco products because of a systemic obstacle. The systemic level strategy that could assist lower the percentage of adult smokers is education about the risks of nicotine and methods for breaking the addiction to nicotine.
References
American Lung Assosiation. (n.d.). Smoke air laws. Web.
Healthy People 2030. (n.d.). Web.
U.S. Department of Health and Human Services. (n.d.). Reduce current cigarette smoking in adults — TU‑02. Web.
Zvolska, K., Pankova, A., Nohavova, I., Huque, R., Elsey, H., Boeckmann, M., Sheikh, A., Siddiqi, K., & Kralikova, E. (2020). A narrative review of facilitators and barriers to smoking cessation and tobacco-dependence treatment in patients with tuberculosis in low- and middle-income countries. Tobacco-Induced Diseases, 18, 67. Web.
