- Introduction
- Hyperlipidemia Among the Elderly
- Hypertension Among the Elderly
- Chronic Obstructive Pulmonary Disease Among the Elderly
- Overview of the Cardiovascular System in Older Adults
- Factors That Contribute to Changes in the Myocardium
- Age-Associated Changes in Arterial Structure and Function
- Conclusion
- References
Introduction
The risk of chronic illnesses such as cardiovascular disease, hypertension, and chronic obstructive pulmonary disease (COPD) rises with age. These are the significant causes of global disease, disability, mortality, and healthcare expenses. On a biological level, aging results from the buildup of several cellular and molecular degradation types. Maintaining healthy behaviors throughout life, including consuming a balanced diet and regular physical exercise, all contribute to lowering the incidence of non-communicable illnesses. The purpose of this presentation is to emphasize how aging is connected with changes in the cardiovascular system. Additionally, it will examine the many health problems that affect older adults, such as hyperlipidemia, hypertension, and COPD.
Hyperlipidemia Among the Elderly
Hyperlipidemias are prevalent, and low-density lipoprotein-Hypercholesterolemia (LDL) plays a causal role in the pathophysiology of cardiovascular disorders like coronary heart disease. Hypercholesterolemia, hypertriglyceridemia, and hyperlipoproteinemia are the most prevalent forms of hyperlipidemia (Rosada et al., 2020). Hypercholesterolemia, characterized by increased LDL-cholesterol levels, is the most well-studied and understood condition, with the most efficient treatments. In addition, there is an agreement about using statins to inhibit atherosclerotic plaque development and recurrence in patients with coronary heart disease and peripheral artery disease (Rosada et al., 2020). Although it is uncertain which therapeutic targets should be explicitly attained in elderly individuals, moderate to high-intensity statin medication seems more beneficial than low-intensity statin therapy.
Hypertension Among the Elderly
Hypertension (HTN) is prevalent among adults and is linked with high morbidity and death rates. HTN is characterized by an isolated systolic or diastolic increase or both. HTN should be frequently evaluated and treated in primary care. HTN is caused by the body’s reaction to external stresses to keep blood pressure within the optimal range for the perfusion of essential organs such as the brain and heart. Adults with blood pressure values between 120 and 139 mm Hg (SBP) or 80 and 80 mm Hg (DBP) are advised to modify their lifestyle (Setters & Holmes, 2017). Recommendations include limiting salt intake, alcohol consumption, weight loss or quitting smoking, and minimizing stress.
Chronic Obstructive Pulmonary Disease Among the Elderly
Chronic obstructive pulmonary disease (COPD) is a chronic lung disorder that causes progressive breathing problems. Emphysema and chronic bronchitis are the two most common types of COPD (Cortopassi et al., 2017). In chronic bronchitis, the airways become irritated, resulting in increased mucus secretion, airway constriction, breathlessness, and coughing. The lungs’ alveoli are destroyed in emphysema, depleting several organs of oxygen. The most prevalent cause of COPD is smoking (Cortopassi et al., 2017). Cigarette smoke promotes oxidative stress, damaging DNA and hastening the degradation of lung tissues. Consequently, COPD may be considered a rapid lung aging disease involving cigarette smoke. The management of COPD focuses on disease prevention, symptom reduction, and an increase in exercise ability.
Overview of the Cardiovascular System in Older Adults
The cardiac system is the primary transport system inside the body. Its primary function is transporting oxygenated blood, nutrients, and hormones to organs and tissues. A healthy and long-lasting cardiovascular system is crucial for longevity, but its performance declines with age, negatively affecting all other organ systems. Age is among the greatest risk factors for cardiovascular disease (CVD) (Paneni et al., 2017). Blood vessels, especially arteries, lose flexibility as the body ages and arterial walls grow stiffer and thicker. The tunica media and tunica intima of big and medium-sized arteries gradually get thicker with advancing age. Blood arteries that are aging may also exhibit variable degrees of calcification.
Endothelium, the most fragile layer of a blood artery, is in close touch with the flowing blood. The endothelium produces irregularly shaped cells as it matures and is frequently thickened by the migration of smooth muscle fibers from the medial tunica. This injury to the endothelium initiates atherosclerosis, the most prevalent type of blood vessel disease (Paneni et al., 2017). Damage to the endothelium initiates atherosclerosis, the most prevalent type of blood vessel disease. Atherosclerosis of the coronary arteries may cause coronary artery disease. Frequently, the fatty plaque ruptures, causing clot formation and myocardial infarction. Similarly, atherosclerosis of the carotid arteries greatly raises the risk of stroke.
Factors That Contribute to Changes in the Myocardium
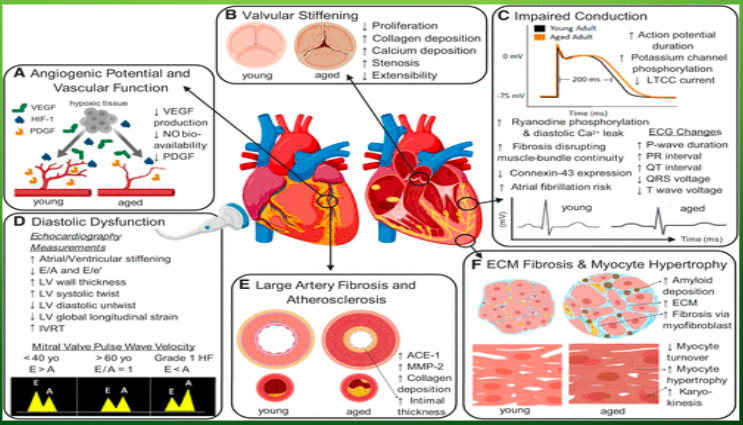
The diameter of the left ventricular (LV) wall rises with age. The hypertrophy of ventricular cardiomyocytes results in part from the increased afterload caused by the stiffness of major arteries (Tracy et al., 2020). In addition, during the aging process, the basal ventricular septum bulges into the left ventricular outflow tract, which is partly due to the reduction in long-axis size and in part due to the rightward shift of the enlarged ascending aorta (Tracy et al., 2020). This modification in form results in a sigmoid septum, a term that describes a bent ventricular septum. This may take the form of asymmetric septal hypertrophy in hypertrophic cardiomyopathy.
The left atrium expands, and the left atrial volume, when adjusted for body size, rises by about 50 percent from the third to the eighth decade, partially accounting for the high frequency of atrial fibrillation in the older population. Similar structural alterations are detected on the right portion of the heart, but they are less pronounced than on the left (Tracy et al., 2020). In a certain Study of Atherosclerosis-Right Ventricle Investigation, there was a 5% reduction in right ventricular (RV) mass for each decade of age. (Tracy et al., 2020). In addition, age-related reductions in right ventricular end-systolic and end-diastolic volumes (ESV and EDV), as measured by magnetic resonance, have been shown.
Age-Associated Changes in Arterial Structure and Function
The vascular system undergoes a variety of age-related structural changes, such as the thickening and dilatation of big arteries. According to echocardiographic investigations, the aortic root vasodilated by about 6 percent during the fourth decade. Chest X-rays have revealed a similar significant increase in the diameter of the aortic knob over time. As early as 1910, autopsy reports revealed age-related aortic thickening (Singam et al., 2019). A variety of functional alterations of the arterial wall media are connected with aging. Collagen and elastin supply the artery wall with strength and elasticity, accordingly, and are typically preserved by enzymatic cross-linking. Age-related increases in collagen composition and collagen cross-linking diminish arterial distensibility and heighten arterial stiffness.
Elderly people are also predisposed to infarction and heart failure due to age-related myocardial alterations. Thickening of the LV wall increases the distance between the epicardial coronary arteries and the subendocardial myocardial cells, hence may cause subendocardial ischemia (Singam et al., 2019). These intramyocardial alterations in capillarity and flow dynamics are exacerbated by arterial stiffness in the periphery. Due to the age-related changes in the vasculature and heart outlined above, which are often exacerbated by long-term exposure to other CV risk factors, hypertension, coronary events, and heart failure become increasingly prevalent with age (Singam et al., 2019). The vasculature’s inherent susceptibility to atherosclerosis predisposes to myocardial infarction, stroke, and peripheral arterial disease.
Typically, electrical remodeling happens throughout the seventh decade of life. The frequency of sinoatrial (SA) node failure with decreasing pacemaker cell density and his-Purkinje system dysfunction (Tracy et al., 2020). Electrocardiogram examinations of older people demonstrate an increase in P-wave length, P-R interval, and Q-T interval, a reduction in QRS and T-wave strength, and a displacement to the left of the QRS wave (Tracy et al., 2020). Reduced peak pulse rate and peripheral oxygen consumption seem to explain the reduction in aerobic function associated with aging. Deficiencies in cardiac b-adrenergic receptor density and the efficacy of postsynaptic b-adrenergic signaling largely contribute to diminished cardiovascular function during exercise in older persons.
Conclusion
Cardiovascular disease (CVD) imposes a substantial cost on older individuals, their caregivers, and healthcare systems. Throughout time, structural and functional abnormalities of blood arteries accumulate, resulting in an increased risk of developing cardiovascular disease. The global increase in the senior population underscores the need to comprehend how aging increases CVD in order to create innovative solutions to address this issue. Alterations to the cardiovascular system are associated with aging. Several health issues, such as hyperlipidemia, hypertension, and COPD, plague older persons. These are the major worldwide causes of illness, disability, death, and healthcare costs. A healthy and long-lasting cardiovascular system is crucial for health and longevity, but its efficiency declines with age, negatively affecting all other organ systems.
References
Cortopassi, F., Gurung, P., & Pinto-Plata, V. (2017). Chronic obstructive pulmonary disease in elderly patients. Clinics in Geriatric Medicine, 33(4), 539-552.
Paneni, F., Diaz Cañestro, C., Libby, P., Lüscher, T. F., & Camici, G. G. (2017). The Aging Cardiovascular System. Journal of the American College of Cardiology, 69(15), 1952–1967.
Rosada, A., Kassner, U., Weidemann, F., König, M., Buchmann, N., Steinhagen-Thiessen, E., & Spira, D. (2020). Hyperlipidemias in elderly patients: Results from the Berlin Aging Study II (BASEII), a cross-sectional study. Lipids in Health and Disease, 19(1).
Setters, B., & Holmes, H. M. (2017). Hypertension in the Older Adult. Primary Care: Clinics in Office Practice, 44(3), 529–539.
Singam, N. S. V., Fine, C., & Fleg, J. L. (2019). Cardiac changes associated with vascular aging. Clinical Cardiology, 43(2), 92–98.
Tracy, E., Rowe, G., & LeBlanc, A. J. (2020). Cardiac tissue remodeling in healthy aging: the road to pathology. American Journal of Physiology-Cell Physiology, 319(1), C166-C182.
