The patient-physician communication quality determines patient experience with healthcare facilities. Both verbal and non-verbal communication techniques need to take into account patients considerations. The Institute of Medicine (IOM) stresses on the importance of using a patient-centric healthcare to improve patients’ satisfaction with treatment (Tzelepis et al., 2014). However, there are a number of external factors which influence patient experience. Some of the major factors affecting patients’ communication and experience with the health sector include age, culture, language, ethnicity, social class, mental health, and literacy level (Burt, Lloyd, Campbell, Roland, & Abel, 2016). Therefore, physicians and support staff need to make careful decisions on the tone and quality of communication used for interacting with the patients.
Effective communication and respect for the choices of patients form the core value of patient-centered care. In this regard, medical professionals and nurses need to develop and follow standard communication processes to ensure patients’ satisfaction. In addition, there is a need to check the quality of patient-physician communication, the performance of which can be measured with the help of process analysis tools. The following are the major types of process analysis tools:
- Flowcharts
- Matrices
- Decision Trees
- Special Diagram
Application of a process analysis tool helps healthcare practitioners to evaluate their performance and provide quality service. In this respect, an effective communication plays an important role. Like other processes, patient-physician communication is also a process. Thus, it is proposed to use process analysis tool to determine the quality of communication and patients’ experience.
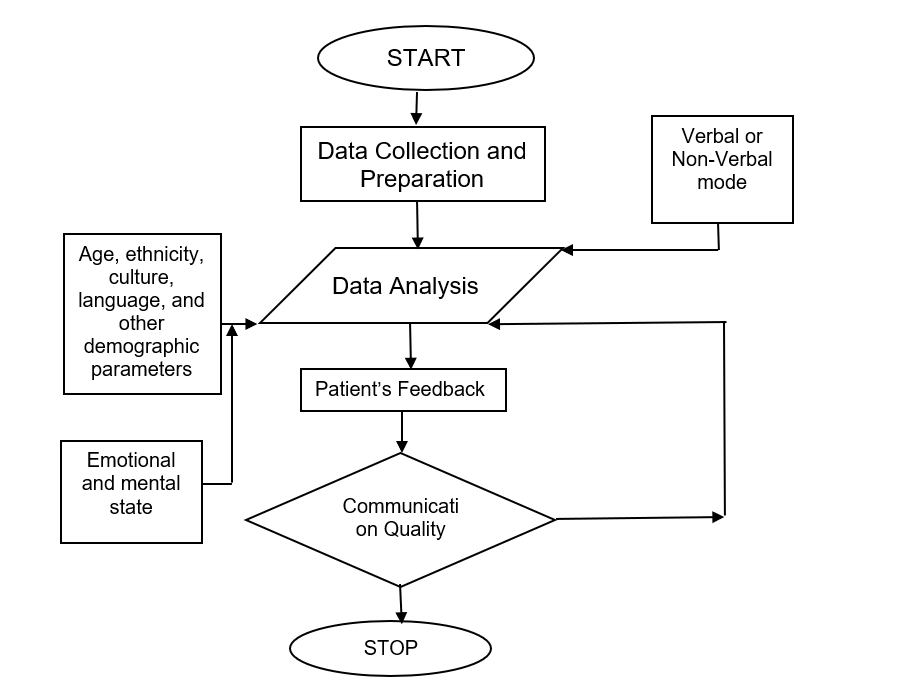
Basic flowcharts can help understand the communication process. Flowchart process tool helps in detail planning, understanding, and improving a given process. For example, the patient-physician communication consists of multiple sub-processes and mediums- the flowchart process tool can demonstrate the relationship between various steps of communication and improve it by suggesting possible root-cause of communication inefficiency and redundancy. Therefore, taking into consideration the above advantage, this work proposes the use of flowchart as a process tool to identify and understand communication process.
Communication Process Tool
Effective communication addresses patients’ requirements and requires proper care plans, treatments, and discussions. The following diagram shows an effective flowchart to improve patient-physician communication by considering important external and internal factors that influence patient experience. Figure 1 suggests that each of the elements plays a vital role in determining the effectiveness of a process. For instance, one needs to consider the environment and mode of communication; in this respect organization, physical environment, technology, task, and diagnostic team members are the important components of communication. The process analysis tool can help improve efficiency and equality issues in healthcare treatment. For example, prior information collection of patients’ demography can help remove ethical, gender, age, and culture bias as reported in many research works (Wong, Gudzune, & Bleich, 2015). Wong et al. (2015) reported that patients’ weight, race, and ethnicity affects relationship and weight of communication between the doctor and patient. For example, black overweight men were more likely to communicate less effectively. Similarly, research works have found that patients’ social statuses also affect the nature of communication.
The effective use of a process tools such as flowchart and root-cause analysis can help collect information about the patient and environment. This intron can help decide mode, tone, and quality of communication to improve patients’ experience in healthcare. The research work shows that advanced process analysis can be used to incorporate technology and help improve decision-making process. For example, the research work suggests the use of content analysis software to improve efficiency and effectiveness of communication between a patient and a doctor. This would help to bring equality into patient experience within healthcare, and remove unnecessary gender, age, culture, and status bias.
All the healthcare activities are based on processes; therefore, process tools can be used to analyse their performance. The process of quality improvement is originally a manufacturing concept adopted from Japanese producers. Nevertheless, the same tools of analysis can be applied to the healthcare sector to analyse and improve performance of various processes. For example, this work demonstrated the use of flowchart as the process tool to investigate and plan patient-physician interactions. The flowchart provides a detail representation of relationship among various elements involved in the communication. Effective implementation of communication in healthcare would improve patients’ perception and impart positive experience for patients of all ages irrespective of language, culture, and ethnicity.
Conclusion
Research works have shown that healthcare practitioners find it difficult to evaluate the performance of patient-physician communication. Inefficient communication between patient and practitioners lead to bias and unequal treatment, which reflects in patient satisfaction level. Therefore, there is a need to effectively monitor and improve the quality of communication which requires multiple considerations such as communication environment, mode of communication, consumers’ demography and other external factors. In this respect, the given work proposed the use of flowchart to analyse the patient-physician communication. This process analysis tool, first, collects data such as environment, communication mode, mental and psychological conditions of a patient. Later the collected data can help make effective decision on the tone and quality of communication. The use of process analysis tool would also help bring equality among the patients’ experience with healthcare. In addition, practitioners can effectively decide on the additional requirements to improve patients experience during the treatment.
References
Burt, J., Lloyd, C., Campbell, J., Roland, M., & Abel, G. (2016). Variations in GP–patient communication by ethnicity, age, and gender: Evidence from a national primary care patient survey. The British Journal of General Practice, 66(642), e47-e52.
Tzelepis, F., Rose, S. K., Sanson-Fisher, R. W., Clinton-McHarg, T., Carey, M. L., & Paul, C. L. (2014). Are we missing the Institute of Medicine’s mark? A systematic review of patient-reported outcome measures assessing quality of patient-centred cancer care. BMC Cancer, 14(1), 41.
Wong, M. S., Gudzune, K. A., & Bleich, S. N. (2015). Provider communication quality: Influence of patients’ weight and race. Patient Education and Counseling, 98(4), 492-498.

