Abstract
This paper presents an exploration of the problem scenario illustrated in the book Code Green. The paper takes a significant thrust on illuminating factors and variables leading to the actualization of the problem scenario encapsulated in the book.
The paper draws evidence presented in the source (Code Green Book) and leverages the synthesis and analysis on various perspectives and insights captured in the various published literature on the problem root scenario and presents feasible propositions on turnaround strategies and ways into the future.
In the write up the possible solutions will be considered and presented in the view of contributing to the alleviation of the problem scenario at BIDMC. The paper culminates in the coagulation of strategy propositions with the aims of making a positive impact on the organizational environment which are of fundamental effect to the entirety of the nursing practice.
Introduction
The book Code Green by Dana Beth Weinberg illustrates in a dramatic sense the deterioration of health care in atypical commercialized hospital entities attributable to the rabid financial inclines of the hospital’s merger owners. Weinberg’s work dramatically captures what is occurring in nursing care between two competitive hospitals, Beth-Israel and Deaconness in Boston which have come together as a merger forming a colossal health care industry.
The title adopted by the author is an aesthetic nuance that serves to denote the precarious situation and looming dangers instantiated by the restructuring of the merger process.
The BIDMC scenario presents a microcosm of the pervasive change sweeping right through the health care system in America prompted by stiffening marketing trends. During the BIDMC eon, many health care entities in the U.S were pushed to the edge of dire financial straits. The crisis was aggravated by escalating health care costs. Harry Jacobs Summers (2005) notes, “Reimbursement rates began to drop as private insurance entities gained power to bargain in the managed care era, and dropped sharply in the wake of the Balanced Budget Act of 1997, which restricted Medicare reimbursement. As a result, the hospital industry increasingly turned to prevailing private sector business practices to cut costs, including consolidation, internal restructuring, and lean staffing. This often meant that fewer nurses struggled to care for more patients.”
The Blow on Service delivery
Following the merger service delivery in the hospital has plummeted such that patients are served with bad food, patients have to remain for hours unattended and when they are attended the service is a shortchange for the value for money and the regard for the sanctity of life. The book explores in profound depth how the nursing profession has undergone drastic transformations in the course of the past decade. The author cites the hospital consolidation and the 1997 balanced Budget Act which led to the instrumentation of certain nursing profession benefits such as Medicare payments resultantly triggering ripple personnel dissatisfaction effects down the hospital’s service delivery system.
The author presents the foregoing as the salient root cause of a plethora of problems dogging the Hospitals, Beth Israel Deaconess Medical Centre (BIDMC). The Brandeis University research associate has used the merger of Boston’s prestigious Beth Israel Hospital with New England Deaconess to illustrate the manner and extent to which financial hurdles as well the vital aspect of consolidation have led to the acute dearth of nurses as well as unbridled discontent in the field.
What must be noted in the transformations that Beth Israel has gone through is the extent to which the merger concept and strategy has transformed the institution which has had to veer off its policy and principles founded on the values and ideology of egalitarianism. On the other end, New England Deaconess has relinquished its well reputable image and its hallmark based on its “Restructuring of Hospital care” thrust in the aims of cost-efficiency.
The fusion of the two institutions’ information of the major merger was an attempt to marry two distinct entities with critical disparities in policy, philosophy, and orientations. The ongoing political grappling exerted negative repercussions on the merger resulting in critical nursing staff turnover and negatively affecting patient care. In essence Code, Green is also an illustration of financial constraints that hospitals are facing in contemporary health care systems. According to The Publishers Weekly (2003) “The Book is a thorough investigation into how the nursing profession has changed radically over the last decade.”
The book presents a multi-dimensional outline of the BIDMC’s woes through its explorations of dynamics obtaining following the merger of the two hospitals. The book can be interpreted as a tribute to the nurses who have to bear the brunt of the extenuating work climate during the restructuring phase of the merger transition. The author also manages to bring into focus comparisons in the aspects of nursing productivity between the fundamental nursing models and other paradigms of nursing in the premise of physician nursing relationships.
The author is not silent on the critical aspect of patient care in the milieu of implications of fiscal constraints and financial management dynamics and challenges that faced the merger.
The merger had to kick off with nominal profit margins with the operational and restructuring strategy adopted and adapted from the business sector. The title denotes the hospital’s code green experience. The Code Green terminology is used in hospital industries to refer to a facility failure that prompts and necessitates instant intervention. Code Green illuminates the menace of market-driven and oriented health care systems that have resulted in compromised and highly assaulted health care systems in which values of patient care and health service optimality have been sacrificed on the altar of financial expedience.
The code green scenario is not an isolated scenario of the health care systems unraveling. The scenario is closely relatable to the sweeping changes recorded in the past decade In the US health care system. additionally, in the past decade, both private and public sector health care institutions have been subjected to significant demands on arresting cost growth.
Health care industry transformations
Dana Beth Weinberg and Suzanne Gordon (2004) present, “The historical roots of these trends relate to the consolidation of purchases of healthcare activities. Increasingly, the purchasing of health insurance and health services, traditionally an individual affair, is now conducted by collective purchases.” The scholars outline that the changes began in the public sector in 1965 with the inception of Medicare and Medicaid. Starr (1982) concur that “Consolidation also took place in the private sector through growth of the health insurance industry as it became increasingly common for employers to purchase as a group to provide health benefits to employees”.
The collective implications of this transformation led to a shift of payment burden from employees. The development of the health insurance industry expanded access to health services whilst also increasing the demand for health services.
Dana Beth Weinberg and Suzanne Gordon (Opcit) underscore that in the transformation phase technological advancement enhanced the capacity of carrying out “new procedures and treatments and further fueled demand. This market environment spurred rapid increase in national health care spending.”
The lucrative payment schemes introduced by institutions like Medicare and Medicaid were aimed at luring health practitioners and hospitals to accept patients of these entities.
“These programmes provided fee-for-service payment for health care.” (Optic)
The result of this change was that health care workers were highly incentivized to do more work whilst the system was not checked and maintained for keeping up to optimum standards of health care.
The Balanced Budget Act (BBA)
In 1997 service the American health sector was further shaken by the Balanced Budget Act (BBA) which was tailored to reduce Medicare expenditures by $115 billion for over five years. The bill also stipulated a $17 billion reduction in projected Medicare hospital payments according to Kuttner (1999).
According to Kuttner, the sticking effect of this bill was the removal of the insulations for hospitals that relied on Medicare payments as a way of catering to their cost discrepancies from controlled care and other insurance arrangements. Hallam (1999) adds, “Reports of losses in the millions of dollars for fiscal year 1999 reveal how close to the bone some of the hospital margins have been cut. As a result, some of the BBA Medicare payment reductions have been reversed or postponed.”
It is easier to explore the operational and strategic orientation of the merger given the motives that led to its formation. The merger resulted from competitiveness and market share as well as sustainability considerations by Beth Israel which was losing significant market share to the big competitor Partners Health Care. Beth Israel made the decision to partner with New England Deaconess Health Care as means to consolidate its position in the market in face of sweeping competition from Partners Health Care.
“The newly formed Beth Israel Deaconess Medical Centre (BIDMC) would be CareGroup network’s flagship hospital, its crown jewel, with 1,257 physicians, 7660 employees and nearly $1 billion in annual revenue. Together these groups would play David to the behemoth Goliath that was Partners Healthcare. Alone they could not compete, but together these CareGroup hospitals thought they might reclaim some of the market share now hoarded by Partners”.
It is clear that this merger was invented in baseless optimism where-in operational capacity and naively envisaged financial flexibility were thought to suffice to the catapult the two hospitals to dazzling heights of prosperity and profitability. The grave error identifiable at the formation of merger is based on the fact that the merger was formed for core reasons of business expedience, particularly market competitiveness albeit at the expense of health service delivery.
Financial Constraints
The much hailed merger that had triggered hopes and anticipation for enhanced operations leveraged on envisaged financial flexibility that would consolidate the hospitals in face of stiff competition dominated by Partners Health Care. Nonetheless not much progress was recorded after the merger process. Richard Saltus and Alec Pahm (1999) note, “Integration and consolidation of the two neighboring hospitals had progressed little by 1999, even making allowances for the sheer logistical difficulty involved in closing down hospital facilities and moving whole departments , the process proved more difficult than initially anticipated.”
The foregoing point to the grim picture painted that by the complex factors affecting the major merger. It was clear that the merger had been invented in myopia that had based the invention of the merger on unwarranted optimism and hence the overlooking of various intricacies pertaining to the feasible modeling and management of mergers of this nature and magnitude.
Escalating Costs
One unexpected inverse play down of the merger was the growth in expenditure against the aims to contact cost growth in health care sectors. The simulation in the new entity’s administrative posts for the medical and surgical specialties exerted enervating pressure on the hospitals as this milieu presented greater expenses than initially envisaged. “Duplications in administrative positions and medical as well surgical specialties burdened the hospital with greater expenses than planned. Under these circumstances BIDMC had yet to realise any of the promised financial returns from the merger” (Opcit)
High Staff Turn over
The resonating plethora of dissonances that ranged from organizational operations up to employee dissatisfaction had grim implications for the merger staff turnover rate. Disechanted workers reacted by resignations at worst whilst those who remained worked in clear attitude of despondency which further crippled the hospital’s service delivery.
Michael Lasandra (1998) states, “Prominent surgeons and physician angry at the way the merger had been handled or displeased with new arrangements left their positions at the hospital, draining its prestige. In may 1998, forty contract anesthesiologists serving the deaconess campus quit en masse in response to contract renewal offer deemed unpalatable”. The critical result of this was that the giant entity was left with the anesthesiologists of Beth Israel campus to cater for both hospitals.
The instances of four unexpected surgical deaths which occurred at the hospital dealt the merger a heavy blow on its reputation. The instances triggered an inquest by the departments of public health. The departments investigated the link to the anesthesiology staffing crisis. “Although no evidence was found linking between the staffing shortage and the deaths, BIDMC suffered negative publicity.” (James Reinertsen: 1998) The report from the government inquest confirmed the resonating notions and suspicion that financial driven hospitals were not evaluated for safety and efficacy.
Geographical Distance
The geographical distances, literal land truly symbolic to the two hospitals different world views and entrenched organizational dissonances posed pervasive challenges on the operations front of the running of the giant hospital. The hospitals remained two autonomous entities despite the much vaunted merger deal which had been made albeit out of misguided prospects of business convenience and expedience.
The distance factor had far reaching repercussions on the day to day and minute to minute operations of the hospitals. It took a twenty minutes walk from one end of the campus to the other and this has critical implications for nursing staff that had to scamper up and about for nursing meeting and other duties.
The distance was particularly a brunt to bear during the unfriendly New England winter. Such seemingly negligible technicalities had critical contributions to the performance on the heath care fronts of the merger. The distance proved to be an inhibitive factor for the prospects of optimal care, effectiveness and efficiency. This variable instantiated one dimension in the “dismantling of nursing” reality.
Operational Dissonances/ employer dissatisfaction
Upon the constraints posed by the geographical distance, it is particularly noteworthy that each campus had its own way of doing things. Crippling variances occurred ranging from paper work, computer systems as well as models of care delivery. “These differences, some trivial, made it difficult for clinical staff to move back and forth across the campuses as needed”
Weinberg and Suzanne (Opcit) note, “A frustrated staff warned that these slight variations could hinder patient care. In an often repeated example, the color used to flag physician orders needing to be filled differed on the two campuses, with the color used on one campus meaningless to another. If a Deaconess Doctor visiting the Beth Israel campus used the usual Deaconess color to flag orders, the orders would be ignored.”
This presents the dire situation that charcterised work activity and operations at BIDMC. The scenario smacked of rivalry and crippling dissonance as workers failed to fuse and work in synch owing much to the unharmonised and somewhat antagonistic work systems of the two hospitals.
The scholars note, “In telling the story, staff members cautioned that this innocent mistake could delay patient care and potentially prove harmful. This trivial decision of which colors to use for flagging orders; a decision that could have been made with a coin toss took two more years to make. Moreover once it was made, the deaconess staff griped that their color system had not been chosen. With growing anger, they complained that they were being forced to do everything the Beth Israel way.”
This illustrates the great chasm that existed in the marriage of these two hospitals which were in essence married but had remained divorced. The scenario was prescient to the looming unraveling triggered by deep seated grievances emanating from cultural differences and power struggles. This heightened the dismantling of the nursing which the authors of Code Green attempt to underscore right through their resource.
Power struggles
The study of dynamics of business merger has brought about valuable nuances that have helped understand and interpret the problem factors and variable around the BIDMC merger. Kantar (1997) indicates that in merges workers view the making of decisions and the further adoption of made decision as signals of power. In this perspective workers in a merger work environment view the decision making process as a win or lose scenario.
Weinberg and Suzanne observe, “In the case of the BIDMC merger, parties from both pre merger hospitals cast decisions about the best ways of doing things in the new hospital as power conflicts. In this context of conflict, power became a win-lose proposition. Every decision about how to perform work could be interpreted as a power struggle in which one side exerted power over the other. The situation rendered some workers powerful and others powerless.” This presents the scenario at BIDMC as untenable.
It vital to note that such challenges are highly likely to have resulted from the fact the merger strategy was invented out of a concoction of borrowed business merger concepts and modeles which were superimposed in negligence of the complexities of the health care sector thus rendering the tie between the two hospitals untenable.
The scholars add, “A zero sum struggle can have serious consequences when it renders individuals powerless to influence decisions.” Needless to say this results in palpable levels of dissatisfaction on the part of the entirety of the hospital staff posing grim implications for health care delivery. Kanter (1997) concurs, “When a person’s exercise of power is thwarted or blocked, when people are rendered powerless in large arena, they may tend to concentrate their power on those over whom they have even a modicum of authority.”
On power struggles dimension Esyllt Jones (2008) adds, “The merger was fraught with power struggles and culture clashes between personnel at the two hospitals. In the case of nursing, the reasons for the clash were plain. Beth Israel’s management style had been consensus-based, relying upon debate and experience to make decisions. By contrast, Deaconess had adopted Total Quality Management (TQM) during a restructuring exercise in the early 1990s, and had a data-driven decision-making style.”
Cultural clashes
Organizational culture is the oil that keeps an organizations running. The giant hospital tailored out of the merger deal needed this as much. Nonetheless the two hospitals exuded significant conservative thrusts as the relics of the pre-merger characteristics surfaced and featured prominently in the new merger dispensation. This triggered cultural clashes right through the running of the show and this had imminent implications for the organization’s efficient and effectiveness aspects and albeit its sustainability.
Weinberg and Suzanne quotes Buono and Bowditch (1989), “Cultural clashes between two mergerring organizations become prominent several months after a formal merger due to the difficulties inherent in integrating employees from two different organizations with different styles, approaches and sometimes mission”.
It would seem that BIDMC committed the common mistake noted from many mergers; that of concentrating on the macro elements of the merger process without paying sufficient attention to the intricacies of ensuring the synchronisation of operational systems and functionalities to ensure seamless systemic progression.
In the terms of Mitehel Marks and Philip Mirvis (1992), “mergers tend to produce an ‘us versus them’ attitude. As a result, workers feel threatened by the new comers’ beliefs and values about the best way of doing things. Such cultural collisions occur even in merger between companies that seem to be culturally similar”. BIDMC had along way to go in optimising the merger process by harmonising all the key factors and variables to ensure efficiency and sustainability.
Organizational proposal
The BIDMC merger has faltered due to a collage of various factors ranging from change mismanagement to superimposition of typically business and non-health-care related organizational structures and change concepts. Needless to say the mergerring process has overlooked the intricacies of the health care system. This is demonstrated by the implementation of the transition process based on concepts and models borrowed from the business world.
It must be noted that these models overlook the distinctiveness of the health care landscape and the implications that it poses for change, mergerring and sustainability. In drafting and charting a perceivably feasible way into the future this section of the paper presents drafted propositions which are based on preferred organizational models for the health entities.
The study has considered the various models available for health institutions delving into the specific tenets of each. Models reviewed include the Rowa model the Kitson model and the Rosswurn and Larrabee model and finally the Advancing Research and Clinical Practice through Close Collaboration (ARCC) model. After a thorough review of available organizational models in the cognisance of other related factors, The Rosswurn and Larrabee model has been adopted for the theoretical and conceptual framework of this proposal although the study presents novel ideas and insights into charting a feasible way out of the BIDMC debacle.
The Rosswun and Larabee Model was crafted within the precincts of theoretical and research literature related to EBP, research utilisation , standard language as well as the critical change theory. Bernadette Mazurek Melnyk et al (2004) indicates, “This model guides the practitioners though the entire process of EBP, beginning with the assessment of the need for change and ending with integration of an evidence-based protocol”
Owing to the feasibility imports of the model, the model has been utilised in primary care scenarios and was adopted a standard of delivery in acute care settings according to Rosswurn and Larabee (1999). Bernadette Mazurek Melnyk et al (Opcit) further state, “Organizations that have adopted this model have done so because nurses in the clinical setting find it easy to understand, possibly because they see the stages of the model as similar to the nursing process”.
Esyllt Jones (2008) asserts, “The greatest difficulty facing Weinberg, and other critics of hospital restructuring, is to establish that what has happened to nursing practice threatens the safety and recovery of patients. Code Green doesn’t provide any data on measures such as medication errors, complications, falls, and so on.” The propositions drafted after this study is aimed at restoring the values of efficiency and effectiveness in the BIDMC health care system.
Jones further points out, “Administrators at BIDMC argue that standards of care remain high, and that patients are satisfied. An inpatient survey, they argue, found 85% patient satisfaction. If you ask nurses, however, as Weinberg did, quality is deteriorating, and the emotional and psychological aspect of healing ignored.” The sticking reality of the scenario which the research endeavor aims to have turned culminates from the fact that health care service providers as well as patients “seem to have lowered their expectation of institutional care. In the process nursing has become a less appealing career for women and the seeds of a nursing shortage are sown” (Esyllt Jones: 2008)
Fig 1 below presents the step of the Rosswurn and Larabee (1999) Model within the Evidence Based Practice (EBP) in nursing framework:
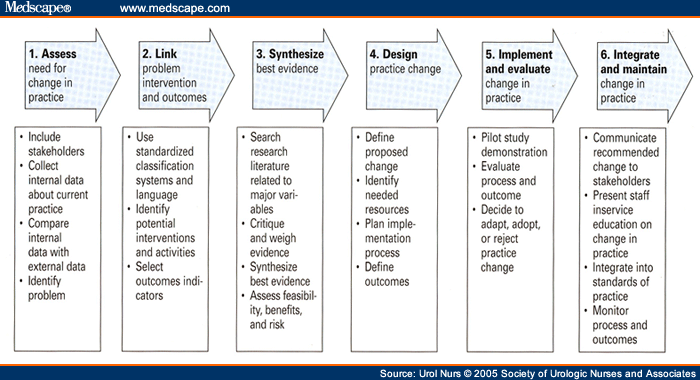
The steps of the models are as follows.
- Asses The Need For Change In Practice
- Line The Problem With Interventions And Outcomes
- Synthesize The Best Evidence
- Design A Change Practice
- Implement And Evaluate The Practice
- Integrate And Maintain The Practice Change.
The proposition drafted in this study draws from the pragmatism merits that have been spawned by the Rosswurm and Larrabee model for health organizations. The proposition has a formidable leverage on the model’s proven framework for empowering clinicians in the processes of evidence-based practice organizational change.
The thrust of the proposition offered in this study is that health care organizational change must entail a holistic and multi-dimensional approach that will bring all variables and factors critical to change process success and organizational sustainability into perspective. This will entail the rigorous liaison with all parties involved, the nursing staff, the stakeholders, the patients who are the key clientele base for typically profitable health care organizations.
The core objective of the thrust will be to familiarize all parties involved with the organizational intent on change and assess change resistance proportions through various research methodologies that will make use of quantitative research tools to draw inferences of critical values in ensuring that health care organizational change process are carried out in synergy.
The propositions made here are in tandem with the fourth and fifth stages of the Rosswurm and Larrabee model presented above. According to Boldreghini, S (1998), “The Design Practice Change is a roundtable discussion which was conducted at the EBNP conference, followed by several other focused discussions about practice changes. Several strategies were identified to explore the original issue further and to implement it into practice. For instance, programs have been implemented educating and mentoring nurses in strategies of detecting early warning signs and communicating these effectively to other members of the health care team.”
On the other end the solution drafting has drawn from the fifth phase is the Implementation and Evaluation of Change in Practice which has shown that, “Currently, the evidence does not support changing practice, but rather building and fortifying systems of knowing the patient, identifying problems early, and communicating and managing changes in patient status in a timely manner.” (Opcit)
These are the fundamental concepts of the solution to the BIDMC debacle. The proposed solutions are based on values of minimising parties’ passiveness in organizational process and ensuring collaboration with stakeholders whilst maintaining acute emphasis on the harmonization of all system units to accomplish success and optimum health care service delivery.
Proposal rationale
The solutions proposed here in have been conceived from a pro-preventative or preemptive approach. Although the Rosswurm and Larrabee model present that there is a yawing gap between the research findings and practice, it is perceived that a problem anticipatory approach will assist in coming up with preemptive measures for instances to curtail the potentialities like resistance to change attributable to work activity dissonances. The BIDMC will have to adopt these suggestions to remodel its commitment on reducing redundancies and increasing efficiency.
The strategy entails long-term planning and strategy implementation in the regard of staff development in tandem with prospects of job enrichment necessitated by a merger. The foresighted organizational process stratagem will eliminate ideological recycling that characterised the initial BIDMC transition which later saw the expanded role of nursing assistants in form of nursing students, a scenario evocative of 1940s where student labour contribution was solicited in the quest to grow health care.
References
Richard Saltus and Alec Pahm, (1999) “BI deaconessStill Feeling Merger pain: Medical Center Morale, reputation Suffer,” Boston Globe.
Michael Lasandra, (1998)Deaths May Be Symptom of Medical Merger Mania, “Boston Herald.
James Reinertsen , M.D, (1998), Address to the medical staff, BIDMC, December 23, videotape.
Larrabee, J.H., (1999), Emerging model of quality. Image – Journal of Nursing Scholarship, 28(4): p. 353-8.
Larrabee, J.H., J.A. Ferri, and M.T. Hartig, (1997), Patient satisfaction with nurse practitioner care in primary care. Journal of Nursing Care Quality, 11(5).
Boldreghini, S. and J.H. Larrabee, (1995), Difference in nursing documentation before and after computerization: A pilot study. On-Line Journal of Nursing Informatics, 2(1).
Hunter, M.A. and J.H. Larrabee, (1998), Women’s perceptions of quality and benefits of postpartum care. Journal of Nursing Care Quality, 13(2).
Larrabee, J.H., L.V. Bolden, and M.R. Knight, (1998), The lived experience of patient prudence in health care. Journal of Advanced Nursing, 28(4).
French, K.S. and J.H. Larrabee, (1999),Relationships Among Educational Material Readability, Client Literacy, Perceived Beneficence and Perceived Quality. Journal of Nursing Care Quality, 13(60).
Larrabee, J.H. and L.V. Bolden, (2001) Defining patient-perceived quality of nursing care. Journal of Nursing Care Quality, 16(1).
Larrabee, J.H., et al., (2001), Evaluation of documentation before and after implementation of a nursing information system in an acute care hospital. Computers in Nursing,19(2).
Rosswurm, M.A. and J.H. Larrabee, (1999), A model for change to evidence-based practice. Image – Journal of Nursing Scholarship, 31(4).
St. Clair, K. and J.H. Larrabee, (2005), Clean vs. Sterile Gloves: Which to Use for Postoperative Dressing Changes? Outcomes Management, 6(1).
Larrabee, J.H., (2004), Advancing quality improvement through using the best evidence to change practice. Journal of Nursing Care Quality, 19(1).
Larrabee, J.H., (2001), Achieving outcomes in a joint-appointment role. Outcomes Management for Nursing Practice, 5(2).
Maramba, P.J., et al., (2004), Discharge planning process: applying a model for evidence-based practice. J Nurs Care Qual, 19(2).
Larrabee, J.H., U.S.,.,(1996) health care revolution: cost and quality challenges, International Journal of Quality Science, 1(2).
Beck, K.L. and J.H. Larrabee, (1996), Measuring patients’ perceptions of nursing care. Nurs Manage, 27(9).
Larrabee, J.H., V.F. Engle, and E.A. Tolley, (1995), Predictors of patient-perceived quality. Scand J Caring Sci, 1995. 9(3).
Larrabee, J.H., (1995), The changing role of the consumer in health care quality. J Nurs Care Qual.
