Introduction
Smoking is a leading cause of preventable death and disease worldwide, causing millions of early deaths annually. Moreover, the adverse health effects of smoking range from acute to chronic conditions, including various types of cancer, respiratory problems, and heart disease. However, nicotine, the primary active ingredient in cigarettes, is highly addictive, leading to dependence and addiction. The thesis of this paper is that smoking is a significant public health concern worldwide, causing extensive morbidity and mortality and contributing to a substantial economic burden on healthcare systems. This report aims to raise awareness of the adverse effects of smoking and promote public health measures to reduce smoking prevalence among adults over 18.
Importance of the Issue
Smoking is a pernicious habit affecting adults worldwide, causing extensive morbidity and mortality. According to recent data, tobacco use contributes to approximately 6 million early deaths annually, making it a leading cause of preventable death and disease (Levy et al., 2021). This number is staggering, underscoring the urgent need for tobacco control measures to mitigate the deadly consequences of smoking. Smoking is a known risk factor for various diseases, including oral cancer, lung cancer, heart disease, respiratory problems, and stroke (Hernández and González, 2020). Acute effects include increased heart rate, elevated blood pressure, and reduced lung function. In contrast, chronic effects encompass several debilitating diseases, including chronic obstructive pulmonary disease (COPD), emphysema, and lung cancer (WHO, 2022). The adverse health effects of smoking are well documented and range from acute to chronic conditions.
The economic burden of healthcare costs associated with smoking is substantial. A recent study found that smoking-related healthcare costs and productivity losses amount to approximately £12.6 billion in the U.K. annually (Hernández and González, 2020). Furthermore, smokers often experience a lower quality of life, leading to decreased productivity, increased absenteeism, and reduced work capacity (Roser and Ritchie, 2022). Therefore, reducing smoking prevalence among adults over 18 is essential to promote public health and reduce healthcare costs.
Individuals Impacts
Smoking is a significant public health concern worldwide, and it has been established as a leading cause of preventable deaths and diseases. In the United States alone, cigarette smoking causes an estimated 480,000 deaths yearly, equivalent to one in five deaths. It results in more deaths each year than HIV/AIDS, illegal drug use, alcohol abuse, motor vehicle injuries, and firearm-related incidents combined (WHO, 2022). Nicotine, the primary active ingredient in cigarettes, is a potent central nervous system stimulant that produces pleasurable sensations, such as relaxation and euphoria, by releasing dopamine in the brain (Roser and Ritchie, 2022). Moreover, nicotine is highly addictive, and it can lead to addiction and dependence, a chronic and relapsing condition characterized by compulsive drug-seeking behavior, even in the face of negative consequences (Roser and Ritchie, 2022). Quitting smoking can be challenging due to the physical and psychological dependence on nicotine (Roser and Ritchie, 2022). It can cause withdrawal symptoms, including irritability, anxiety, depression, restlessness, and difficulty concentrating, lasting several weeks or months.
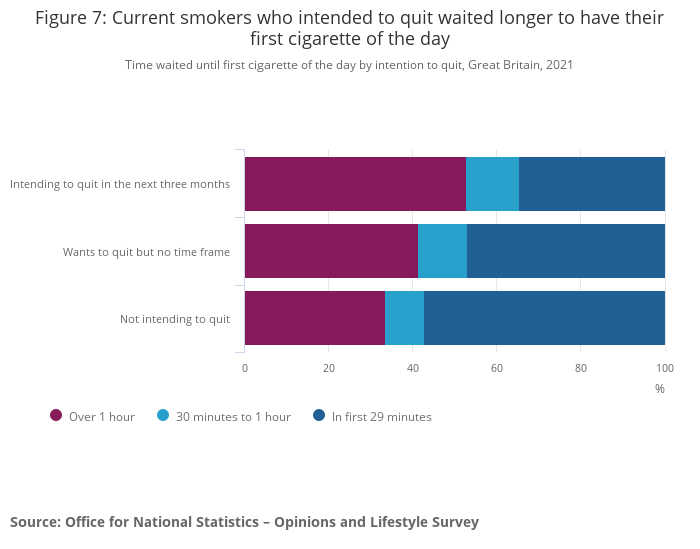
According to a survey, 55.3% of smokers have expressed their desire to quit smoking. Out of these, 21.7% plan to quit smoking within the next three months. However, the survey also reveals that individuals who intend to quit smoking tend to delay smoking their first cigarette of the day (as seen in Figure 1). Specifically, of those planning to retire within three months, 47.2% smoked their first cigarette within an hour of waking up, while 66.5% of those with no intention to leave smoked their first cigarette within an hour of waking up.
Furthermore, smoking can also cause respiratory problems, such as bronchitis and pneumonia, and it can worsen asthma symptoms. Lung cancer is the leading cause of cancer death in the United States, and cigarette smoking is responsible for about 85% of lung cancer cases (WHO, 2022). Smoking can have detrimental effects on reproductive health and pregnancy outcomes. For instance, smoking during pregnancy increases the risk of premature birth, low birth weight, stillbirth, sudden infant death syndrome (SIDS), and respiratory problems in infants (Roser and Ritchie, 2022). Secondhand smoke exposure can also cause respiratory problems, such as asthma and bronchitis, in children (WHO, 2022). Lastly, smoking can lead to social isolation, as smoking is becoming less socially acceptable and prohibited in many public places, such as restaurants, bars, and parks (Roser and Ritchie, 2022). Moreover, smoking is associated with stigma, leading to discrimination and isolating smokers from social activities and opportunities.
Societal Impacts
The negative impact of smoking on society extends beyond individual health effects and includes a significant economic burden. Moreover, the World Health Organization estimates the global financial burden of smoking-related healthcare costs and productivity losses is over $1 trillion annually (Hernández and González, 2020). In the United States alone, smoking-related healthcare costs are estimated to be over $300 billion annually, including direct medical expenses and lost productivity (Hernández and González, 2020). The environmental impact of smoking is also a concern. Cigarette butts are the most common form of litter globally, and they can take up to 10 years to decompose, releasing toxic chemicals into the environment (Hernández and González, 2020). The burning of tobacco releases over 7,000 chemicals into the air, many of which are toxic and carcinogenic (Yang and Dong, 2019). Smoking produces harmful emissions that contribute to air pollution and climate change.
Smoking can also have social consequences, including stigmatization and discrimination against smokers. In many countries, smoking is becoming less socially acceptable, and there are increasing restrictions on where smokers can smoke. However, this can lead to social isolation and exclusion for smokers, particularly in public spaces (Yang and Dong, 2019). Furthermore, smoking can lead to workplace problems, such as increased absenteeism and decreased productivity due to smoking-related illnesses.
One initiative that has successfully reduced smoking prevalence is the implementation of tobacco-free policies in workplaces and public areas. These policies prohibit smoking in certain areas, making it more challenging for smokers to indulge in their habit and reducing the amount of secondhand smoke exposure to non-smokers (Patanavanich and Glantz, 2020). Additionally, anti-smoking campaigns have effectively reduced smoking prevalence by increasing public awareness of the adverse effects of smoking, promoting smoking cessation resources, and encouraging smokers to quit (WHO, 2022). Furthermore, pharmacological interventions such as nicotine replacement therapy (NRT), bupropion, and varenicline have effectively treated nicotine addiction and aided smoking cessation (Levy et al., 2021). In addition, counseling and behavioral therapies have also been effective in helping individuals quit smoking and maintain abstinence (WHO, 2022). While there are various approaches to addressing smoking prevalence, a combination of tobacco-free policies, anti-smoking campaigns, pharmacological interventions, and counseling and behavioral therapies has effectively reduced smoking prevalence and aided smoking cessation.
Addressing the Issues
The issue of smoking prevalence among adults older than 18 years old is being addressed through various initiatives and policies. The World Health Organization has developed the Framework Convention on Tobacco Control to help countries reduce tobacco consumption and its adverse effects (WHO, 2022). The FCTC includes various measures, such as increasing taxes on tobacco products, banning tobacco advertising, and promoting smoke-free environments. Additionally, healthcare professionals, including nurses, are significant in promoting public health and reducing smoking prevalence among adults. Nurses provide education and resources to individuals, families, and communities and serve as case managers and community consultants.
Alternative Approaches and Recommendations
Addressing smoking and its impact on public health should be taken seriously. The adverse effects of smoking on individuals and society are extensive and well-documented, including physical health problems, such as respiratory problems, heart disease, and cancer, which can lead to premature death. Smoking also has economic costs in terms of healthcare expenditures and lost productivity. In addition, smoking has environmental impacts, as cigarette butts are an effective form of litter, and smoking contributes to air pollution and climate change. Furthermore, social isolation and stigmatization are associated with smoking, leading to discrimination and exclusion of smokers. To mitigate the devastating consequences of tobacco, measures such as anti-smoking campaigns, cigarette taxes, smoking bans, and providing smoking cessation programs should be implemented (Levy et al., 2021). Ultimately, the promotion of tobacco control measures and public health initiatives must be prioritized to reduce smoking prevalence and its negative consequences on individuals and society.
Current approaches to reducing smoking prevalence have succeeded, but they lack personalization and accessibility. Virtual reality therapy is an innovative idea that can be adapted to help smokers quit by simulating the negative consequences of smoking and providing a safe environment to practice coping strategies (Keijsers et al., 2021). Personalized interventions, such as genetic testing and digital tools, can increase the success rate of smoking cessation. Limited access to smoking cessation resources, especially for low-income and marginalized populations, is a significant shortcoming of current approaches (Roser and Ritchie, 2022). Community-based interventions, offering free or low-cost resources, and incorporating smoking cessation into routine healthcare visits can increase accessibility to help and support for smoking cessation.
Conclusion
In conclusion, smoking is a pernicious habit that causes extensive morbidity and mortality, making it a leading cause of preventable death and disease. Furthermore, smoking has detrimental effects on reproductive health and pregnancy outcomes. The economic burden of smoking-related healthcare costs and productivity losses on society is also substantial, leading to a significant global financial burden. As future healthcare providers, medical students must proactively promote tobacco control measures to improve public health and reduce healthcare costs. It is essential to address the devastating impact of smoking on individuals and society by fostering tobacco control measures to mitigate the deadly consequences of smoking.
Reference List
Davies , B., and Revie, L. (2022). “Adult smoking habits in the UK: 2021.” Adult smoking habits in the UK – Office for National Statistics. Web.
Hernández, F.F. and González, E.S. (2020). “The smoking economic control across the primary health services.” Clinical Reviews and Clinical Trials, 2(2). Web.
Keijsers, M., Vega-Corredor, M. C., Tomintz, M., and Hoermann, S. (2021). “Virtual reality technology use in cigarette craving and smoking interventions (i “virtually” quit): Systematic review.” Journal of medical Internet research, 23(9), e24307. Web.
Levy, D.T., Tam, J., Sanchez-Romero, L.M., Li, Y., Yuan, Z., Jeon, J. and Meza, R. (2021). “Public health implications of vaping in the USA: the smoking and vaping simulation model.” Population Health Metrics, 19, pp. 1-18. Web.
Patanavanich, R. and Glantz, S.A. (2020). “Smoking is associated with COVID-19 progression: a meta-analysis.” Nicotine and tobacco research, 22(9), pp. 1653-1656. Web.
Roser, M. and Ritchie, H. (2022). ‘Smoking.” Our World in Data. Web.
Selby, P., Voci, S., Zawertailo, L., Baliunas, D., Dragonetti, R. and Hussain, S. (2018). “Public health impact of a novel smoking cessation outreach program in Ontario, Canada.” BMC public health, 18, pp. 1–11. Web.
World Health Organization (2022). “World Health Organization.” Who.int. Web.
Yang, B.Y. and Dong, G.H. (2019). “Tobacco smoking in Asia—a public health threat.” JAMA Network Open, 2(3), pp. e191471-e191471. Web.
