Reimbursement
Reimbursement is a term commonly used in healthcare and as an alternative name for compensation. Often, clients are reimbursed for services rendered once they have acquired them (Freidson, 2017). Health care is a reimbursable service, primarily since physicians and healthcare facilities cannot reject clients if they are experiencing a real emergency and due to the fact that the details of the service are often unknown beforehand. Healthcare providers would not operate wholly or effectively if patients obtained services but failed to pay in exchange for services rendered. Hospitals depend on insurers to compensate them for patient services to pay their daily expenses, purchase the materials they need, and pay clinicians and staff to run the facility and attend to patients.
Flow Cycle – Patient to Payment
The revenue cycle begins when a client schedules a consultation and proceeds until complete compensation is received. Whereas every facility’s revenue cycle flow is distinct, several essential aspects are always constant. In general, the Revenue Cycle Management Processes entails several elements as shown in figure 1 (Derricks, 2021). Undoubtedly, the labels of the sections will differ across institutions. However, the overall substance of every element will remain consistent. Even so, a few process charts are considerably more comprehensive than some (Derricks, 2021). These several components of the hospital billing process can be summarized under the following parts: Pre-claim, front-end, transactional, and back-end efficiency.
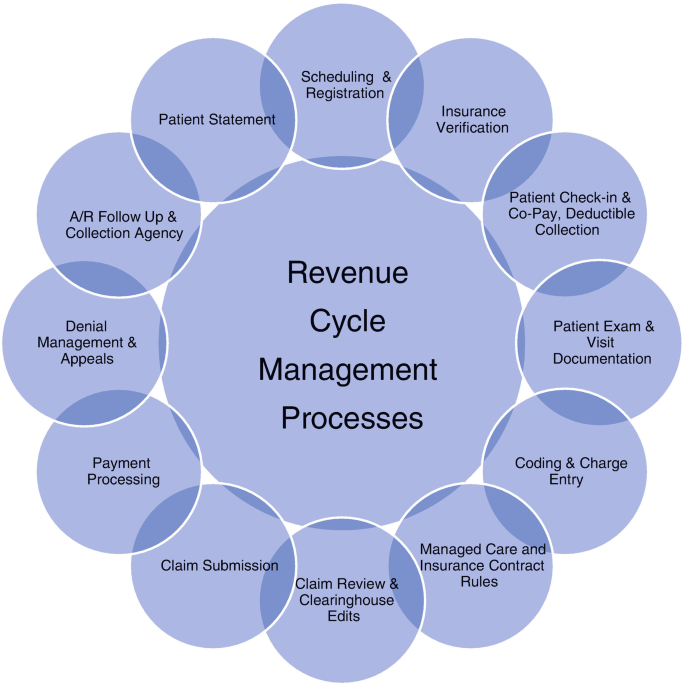
Note. The Revenue Cycle Management Process begins when a client requests services and proceeds until final compensation is received. Though each institution’s medical income cycle is unique, several essential aspects stay constant. These processes can be summarized into five main parts.
Pre-Claim
The component of the healthcare income process does not involve many activities. Instead, it includes things such as provider credentialing and contract negotiations. This part consists of the certification of providers and contract discussions. Similarly, it covers registration for Electronic Data Interchange (EDI) and Electronic Remittance Advice (ERA), as well as the hospital’s pricing and cost structure (Freidson, 2017). The two are crucial for corporate governance and settlement filing. These features make this phase an integral component of the revenue cycle.
Front End
The front-end aspect starts with an initial consultation and ends when the patient leaves. Patients’ enrollment, co-payments, coding, and billing collection are all included. The bulk of the medical revenue stream hinges on this step. Usually, a client’s contact details are recorded, and insurance status is confirmed, including deductibles (Freidson, 2017). A cash flow procedure that follows high standards provides repayment alternatives for whatever remaining debt might not be insured.
Transactional
The transactional segment encompasses nearly every aspect, from cost input to cash reconciliation. In addition to updating reimbursements, it covers claim scrubbing and Electronic Funds Transfer (EFT) processing (Freidson, 2017). Here, rates, claims, and compensation for the offerings are recorded in the database. These many activities make this stage the most important in the flowchart. Mistakes may lead to significant losses for a hospital, culminating in delayed claims or rejected payments (Freidson, 2017). The transactional component is equally critical to statutory mandates.
Back End
Checking claim status, client reports, and claim rejection analysis are part of the back-end element. Reported claims can be resubmitted, and customers must be approached to collect any amounts due. According to Freidson (2017), individuals that decline to compensate can be referred to collections or be subject to complaints. It should be noted that this is the stage in which extra income is collected outside of the transactional area.
Efficiency
A well-functioning revenue cycle increases income, enhances compliance with rules, and lowers expenses. It moreover guarantees that an entity receives the highest possible for its services (Freidson, 2017). A healthcare revenue cycle assists managers in identifying bottlenecks in the system. This way, it enables them to focus on particular aspects of the accounting system that require optimization (Freidson, 2017). Healthcare revenue processes are getting more complicated, demanding a new strategy. Thus, using key performance indicators and quality management standards is necessary.
Departmental Impact on Reimbursement
Data governance in healthcare is the act of storing, safeguarding, and evaluating data collected from various sources. Health systems can construct comprehensive perspectives of patients, customize treatments, establish contact, and improve health effects by managing the abundance of accessible patient records (Melling, 2017). There are two types of audits: the evaluation of standards process and the audit of a submitted claim. In the standards protocol review audit, the practice determines if the practices and processes are relevant and thorough. In contrast, during a claims submission audit, health files and invoices are examined for conformity with coding, invoicing, and paperwork criteria (Freidson, 2017). Medicare’s value-based programs are intended to enhance the efficacy of care, minimize re – hospitalization and the occurrence of care facility illnesses, and transition payouts from quantity (Melling, 2017). Likewise, it entails creating value by monetarily encouraging health personnel for clinical outcomes and efficiency, rather than just the quantity of labor they perform. A value-based pay-for-performance approach compensates physicians for delivering treatment that has been shown to enhance health benefits and incentivizes them to reduce wastage wherever feasible.
It is evident that the revenue cycle comprises several complex elements and that various personnel assist in maintaining that process. For example, patient enrolment, appointment booking, payer contracts, coding, bill recording, claim to file, accounts receivable check out, and denial handling fall within the many components of the income cycle (Freidson, 2017). Therefore, I would ask for records from the billing department to determine which insurers are expected to pay. These records should enable me to distinguish between insured and non-insured treatments or services. Further, I need to review the organization’s charging procedures to ensure that the accounting staff follows stipulated guidelines. Additionally, I would double-check that all services correspond to the charges.
The Health Information Management department is in charge of monitoring for adherence to coding and billing guidelines. Most inpatient clinical information is handled in this division. All doctors are queried about the paperwork of the client’s ailment and the medication they have obtained by a coding specialist. Once this process is completed, the statement is submitted to the finance unit for payment processing (Freidson, 2017). The system will fail if each procedure is not performed in the correct sequence. In addition, if the codes are incorrect, the hospital’s claim will be deferred or declined. Ultimately, it will reflect poorly on the staff and organization.
References
Derricks, J. (2021). Overview of the Claims Submission, Medical Billing, and Revenue Cycle Management Processes. In: Szalados, J.E. (eds), The medical-legal aspects of acute care medicine. Springer, Cham.
Freidson, E. (2017). Professional dominance: The social structure of medical care. Routledge.
Melling, J. (2017). Preparing for value-based payment: fundamental change that encompasses the revenue cycle. Healthcare Financial Management, 71(5), 60-67.
