Background
Project Title
Reducing Patient Falls Caused by Dehydration in Residential Care Facilities: A Six-Month Quality Improvement Initiative
Aim of the Proposal
One of the most significant issues caregivers encounter is morbidity among nursing home patients (Lacey et al., 2019). Falls affect one in three residents of nursing homes in Scotland who are over 65 (Grill et al., 2021). According to Grill et al. (2021), over 18,000 instances are often recorded daily in Scottish hospitals owing to a variety of causes, including infection, contagion, severe disorientation, and dehydration. By introducing fall prevention measures, including hydration methods, educating caregivers, and closely evaluating progress in Scottish nursing homes, this idea seeks to decrease patient falls. The patient’s quality of life will be significantly improved by reducing the number of falls and enhancing their well-being.
In order to lower the risk of falls, this QIP attempts to create preventative strategies to decrease falls. According to research by Lacey et al. (2019), dehydration accounts for more than 37% of falls in nursing homes. There will not be as many waterfalls in the future once measures to enhance hydration are put in place. Increasing hydration will result in a reduction in falls, as this study will investigate the connection between falls and dehydration. Dehydration can cause symptoms including weakness, dizziness, and disorientation, which can lead to a patient falling (Volkert et al., 2019). Dehydration also produces muscular cramps and spasms, which throw patients off balance.
Additionally, it should be emphasized that dehydration is linked to a cognitive imbalance, which makes it difficult for a person to react to environmental dangers that might cause falls (Grill et al., 2021). Vision is a crucial sense that facilitates interaction with the world. Dehydration makes it harder for a person to engage with their surroundings, which affects their capacity to see (Nagae et al., 2020). The idea also seeks to investigate methods of lowering dehydration, which might afterward have an impact on falls.
Every three months, the effectiveness of the suggested actions will be reviewed to see if the number of falls has decreased. To determine if the actions have influenced nursing home patients, an efficacy checklist for hydration practices will be given. If people are taught hydration practices, there will be fewer falls among nursing home patients.
SMART Goal
Implementing fall prevention measures, including hydration techniques, caregiver education, and close monitoring to gauge progress, can reduce patient falls caused by dehydration by 12% over six months.
Research Evidence to Support the Proposed Change
To keep residents safe, hydration techniques are frequently utilized in Scottish nursing homes (Croneri, 2022). The suggested approach will be used differently when the hydration campaign is run by a team that will inform the locals and solicit their input. According to research by Nagae et al. (2020), patients over the age of 65 are considerably affected by falls in terms of psychological stress, bodily damage, and diminished independence. Dehydration in patients causes more than 37% of falls in healthcare settings (Lacey et al., 2019).
Keeping hydrated is one of the most crucial methods to prevent falls. Dehydration causes exhaustion and weakness, which impairs older people’s ability to balance, according to a study by Liu et al. (2019). There is also a link between dehydration and falls in clinical settings, which presents a serious threat to the future of healthcare (Toots et al., 2019).
Another element of this link is that older persons in care use a variety of drugs, some of which have the adverse effect of dehydrating the body. Increasing fluid intake and vigilant monitoring might enhance results in senior housing facilities (Liu et al., 2019). In order to avoid falls and other accidents in care facilities, it is the responsibility of caregivers to guarantee hydration. Improving people’s quality of life and preventing falls are both positively impacted by lowering dehydration. The information provided suggests that more hydration prevents falls.
In order to maintain stability and balance in the human body, the brain is crucial. Research by Li et al. (2019) found that dehydration affects brain perfusion, which lessens flexibility, making it simple for the person to stumble. According to a randomized controlled trial, more than one-third of individuals who fell in nursing homes were dehydrated. Dehydration is a risk issue for older adults over the age of 65 because of aging-related variables. However, diligent monitoring and appropriate care are likely to prevent dehydration and enhance the quality of life (Castaldo et al., 2020).
To lower the danger of patient falls, several of the most effective medical facilities have created hydration programs. It is crucial to know that the likelihood of dehydration frequently occurring in those over 65 will likely increase their risk anytime they become dehydrated. Hydration typically prevents patients from falling and enhances their quality of life (Gulka et al., 2020). In these settings, better hydration services provided by nursing homes lower the risk of falls and enhance patients’ quality of life.
Human health, especially for adults, depends on vision and its clinical repercussions. People can engage with their surroundings more successfully when they have clear eyesight. The level of hydration in the human body has a crucial impact on how well a person can interact with their surroundings (Lee et al., 2019). The danger of falling increases when the body’s fluid levels drop because dry and itchy eyes make it difficult for the patient to see (Edmonds et al., 2021).
When hydration is compromised, the effects of falls are greatly impacted on all levels of functioning, including physical, psychological, cognitive, and visual. However, when medical professionals prioritize hydration, society as a whole benefits (Ree & Wiig, 2019). Therefore, the study will suggest a means of improving hydration, as it is the first step towards reducing falls in a hospital setting.
Identification and Involvement of Stakeholders
Each stakeholder is crucial to the success of the project; hence, stakeholder analysis is vital. Improved regional services are needed in order to increase hydration levels and lower the risk of falls in healthcare settings. The primary parties affected by the amended plans are nursing home residents, employees of these institutions, and regulators.
All nursing home staff will collaborate, and all techniques will be effective if they are all aware of the project. Employees can be encouraged through increased salaries and pay bonuses if they adhere to the changed plan. Nursing staff, therapists, and medical practitioners who deal directly with residents can be identified as critical components in this regard. Through appropriate instruction on all measures to be done to lower the risk of falls in the care facility, caregivers are engaged (Reber et al., 2019).
Staff who are informed and empowered will guarantee that facility residents have access to necessary fluids and keep dehydration-related falls under tight control. Families in need of care are significant stakeholders who ought to be included in the approach. Dehydration rates, for instance, are expected to drop when senior citizens are informed about the advantages of fluid consumption and where they may acquire it.
Another significant stakeholder in nursing settings is the residents of the community. As a part of the project, they have to be well-informed on how to remain hydrated in every location. In this regard, regulators and medical professionals like doctors and nutritionists also play a crucial role by ensuring that the proper hydration levels are maintained in the facility. The competency of hospital employees will be monitored by regulators (El-Sharkawy et al., 2020). If these parties are properly involved, there may be more options for care within the facility.
Suppliers of food and beverages are an essential component in ensuring that the necessary fluids are delivered in the proper kind and amount (Llorens-Gámez et al., 2020). To get the most significant outcomes throughout the conversation, it is essential to ensure that each designated stakeholder is aware of their position (Kavouras, 2019). Therefore, it is the responsibility of the researcher and project manager to make sure that all stakeholders are informed of the changes that are occurring and motivated to improve.
Quality Improvement Tool to Utilize
A quality improvement tool called a driver diagram will be used to graphically describe a problem and suggest necessary improvements (NHS England, 2022). A tool should be utilized to ensure that progress is recorded and feedback is obtained as initiatives to minimize falls by reducing dehydration are adopted. All stakeholders may better grasp the issue and the drivers that can be used to resolve it by using the driver diagram (Llorens-Gámez et al., 2020).
This technology is crucial because it enables the project team to examine and address each component individually. The activity can be tracked more easily, and stakeholders may participate in the problem-solving process when it is broken down into drivers, thus providing a more straightforward path to solutions. The driver diagram helps to organize the steps that need to be performed to solve the fall problem, as illustrated in the figure below.
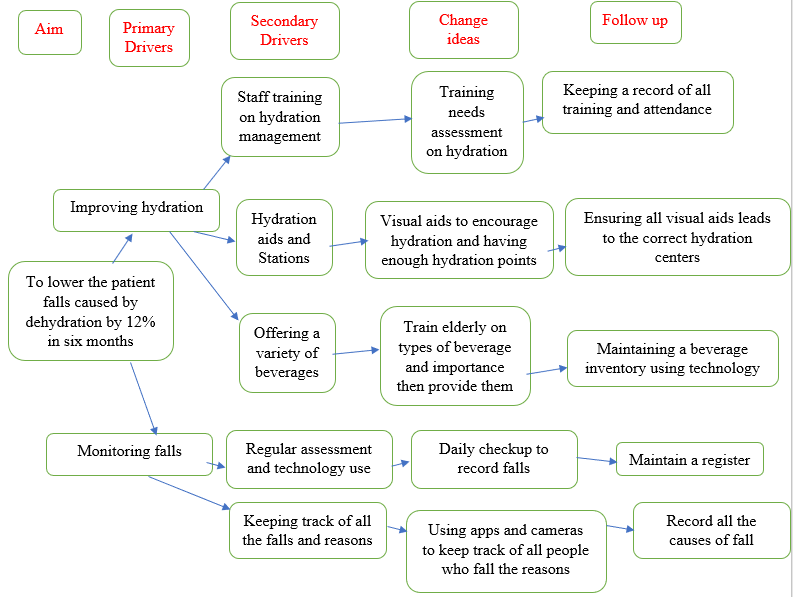
Driver analysis, as its name implies, aids individuals in identifying the underlying cause of any issue so they may find a remedy. This will lead to falls being countered due to dehydration. It is significant to remember that this tool is helpful for communicating ideas since it offers a visual representation that aids in the audience’s better understanding of the issue.
The suggested driver diagram ensures that the dehydration issue is handled and that all causes are studied in an integrated way, delivering a solution. It is an organized approach to the project. To enable teams to collaborate in a multi-frame manner, share ideas, and discuss solutions to patient-related problems, this driver diagram will be employed in this project (Perrier et al., 2021).
Breaking the issue down into smaller parts will help the project since it will give insight into the precise regions where the suggested efforts will be focused. For instance, it can aid in building trust with community residents and provide a better quality of education on dehydration. This diagram can assist a project in producing better outcomes in countering falls due to dehydration.
Furthermore, the tool’s communication feature will make sure that everyone working on this project has all they need to succeed. This will make it possible to construct and evaluate cooperation because it works best when members can successfully interact and exchange ideas (Watanabe et al., 2020).
Consequently, this tool will be crucial to ensuring that everyone receives accurate and trustworthy statistics, data, and other vital information regarding the Scottish systems’ stakeholders. The chosen tool will also assist the team in concentrating on executing the selected dehydration prevention measures across the nation, making sure that all stakeholder data, a health facility analysis, and other aspects are taken into consideration.
Measures of Improvement
The key goal of the proposal is to ensure that the number of falls results from dehydration. However, measures need to be taken to ensure that the initiatives are progressing in the discourse. Some of the measures include the number of falls, hydration levels, and the knowledge given to the staff. When the measurement records a change in the positive trajectory, it means that people can lead better lives.
Measurement Plan
Baseline and Outcome Measures
A baseline measure for the project will be fall rates within the last year collected by the statistical data centers. Through the project, the record of falls will be taken daily alongside the hydration posters put in place. After a week, the falls will be compared to the previous data. This is essential to ensure the necessary changes within a fixed timeline (Gulka et al., 2020). When the number is lower, it will mean that the initiative is making progress.
Process Measures
Hydration level is an important measurement that reflects the caregivers’ efforts to lower falls, among other factors. When the efforts are not successful and the hydration levels are low, the team is mandated to ensure that all the people in the care facility receive appropriate care. Improvement will be recorded when the hydration levels increase, and the number of dehydrated patients lowers (Reis da Silva, 2023). An increase in the number of cases of dehydration should lead to more initiatives to address the problem.
Balancing Measures
The staff plays a significant role in lowering dehydration levels and reducing falls in the hospital setting. The project manager’s responsibility is to ensure that all the people dealing with the patients have the correct knowledge and skills to take care of them (Lacey et al., 2019). This will ensure that they always maintain a higher hydration level.
Satisfaction Level Among the Residents and Their Families
Nursing home residents are delighted when falls are fewer and dehydration levels have improved. In contrast, they are unhappy when falls increase (Perrier et al., 2021). These statistics are worth considering to reduce dehydration levels, thereby improving patients’ quality of life.
The Process to Generate an Improvement
Quality improvement initiatives can be associated with a precise process that can improve the process (Hamrick et al., 2020). All initiatives to lower falls must also be keen to lower dehydration, since it is a prerequisite for reducing accidents. The Plan Do Study Act (PDSA) technique ensures that a challenge is understood and a planned initiative is proposed (Perrier et al., 2021). The data collected will be used to study the trend, and a better method of improvement will be proposed. Once the study is completed, a person can act based on the results. The data collection will be done using the qualitative method.
All measurement choices will successfully employ the PDSA cycle to guarantee that hydration levels rise and that dips brought on by dehydration are minimized. A crucial strategy that is likely to enhance the quality of life is the regular monitoring of hydration consumption. A recording and monitoring strategy will provide a rough picture of the facility’s fluid consumption since greater fluid intake enhances hydration. The level of falls will be removed after it is updated.
Additionally, patient education will have a significant role in determining fluid intake and hydration levels. The standard of medical treatment in the institution will be raised to provide better outcomes in the future when the level of training is taken into consideration, and any observed deficiencies are acknowledged as a necessity for education. Nutritionists will be employed in action plans to instruct patients on appropriate hydration consumption.
To address each person’s hydration demands, individual care plans are crucial. Due to numerous aging hormones, people over 65 are likely to encounter hydration issues (Perrier et al., 2021). Dehydration, however, cannot be permanently resolved in the absence of individualized programs since it is impossible to utilize generic drugs or drinks to increase hydration (Perrier et al., 2021). To ensure that everyone is working hard to improve customized care in nursing homes, the study results might be auctioned off. The significance of special care will undoubtedly become more apparent if the PDSA plan is not used, and ultimately, individuals will be able to satisfy everyone’s demands.
An essential strategy to boost hydration levels and guarantee that patients in a healthcare setting are at the proper levels is to monitor patients’ levels of hydration routinely. The course of action will depend on people’s levels of hydration, and the more falls that are drastically decreased, the more people get hydrated. All suggestions provided following measurements are likely to enhance the standard of living for senior citizens residing in a care facility.
In order to lower levels of dehydration, this initiative will employ posters to inform all inhabitants about the hydration strategy. Posters advising patients to drink more water will be made more visible and adapted to the requirements using the PDSA. Residents will have the chance to give thoughtful comments on the posters’ success in promoting hydration and preventing falls three months after they are up. To ensure that every resident gets adequate information, the technique of putting up posters will be changed, if nothing else.
Implementation Strategies to Sustain the Changes in the Long Term
Posters and other project-recommended activities, like improving patient education, are going to help with hydration. The variety of residents in nursing homes, each with varied requirements, can eventually cause dehydration and falls (Hamrick et al., 2020). As a result, the project’s goal is to make sure that better methods of addressing all dehydration-related risks are created. Variety in fluids offering, employing hydration aids, and putting hydration policies in place in facilities are a few of the techniques.
A key strategy for encouraging individuals to drink adequate fluids within this stage of the project is to provide a choice of drinks. Due to their urinary habits, older persons frequently decline fluids (Lacey et al., 2019). However, the plan makes sure that people are tested for nutrition, and nutrition specialists identify which fluids consumed at the facility not only have nutritional value but also have a likelihood of producing superior results. Fluids have an impact on dehydration levels by making diets more straightforward and by ensuring that the body gets adequate fluids.
This project aims to ensure that people are continually reminded to drink the correct amount of fluids to keep their bodies hydrated via hydration posters. People in a facility are more likely to improve their health and enjoy better lives when they have access to fluids (O’Kane et al., 2020). Institutional visual aids that motivate patients and their families to drink more water will probably yield better outcomes and will probably make people live longer and healthier lives (Ree & Wiig, 2019).
The best outcomes from a conversation are those that evaluate the efficacy of hydration products (Reis da Silva, 2023). People’s hydration levels will increase with the introduction of a hydration-supportive visual aid, resulting in project success. The project’s success depends on the implementation of a hydration regimen since it guarantees that patients receive the proper medicine. A healthcare facility uses a series of list procedures to make sure that its patients are properly hydrated at all times (Reis da Silva, 2023). Hydration guidelines may be evaluated periodically to guarantee that everyone using the facility is safe and getting enough water to provide the best outcomes possible.
Plans for Dissemination
Disseminating learning is essential in the healthcare domain because it helps to offer best practices in the discourse. Sharing best practices is considered an antidote to better health because it provides better outcomes (Reis da Silva, 2023). Dissemination helps improve the culture of quality improvement, making people yearn for better outcomes in the healthcare domain. Accountability and support can be obtained by sharing the research information because a person who gives out information may get the required support (O’Kane et al., 2020).
In the provided settings, when people know that they are to disseminate the information after research, they are likely to be more creative and accountable as they strive to deliver better services. Dissemination of learning is the antidote to improving the quality of life because sharing the best practices is likely to make people lead better lives. Different people within and outside the organization are interested in the project. Insiders include the patients, their families, and residents.
On the outside, the people interested in the quality improvement program include the regulators who are mandated to take care of patient falls. Whenever people understand the quality improvement program, they are likely to offer comprehensive regulation (Kim et al., 2023). The project will be communicated to the members of the public and the patients through a memorandum to make them aware of the findings, which can benefit the healthcare facility’s approach to patient care.
Reference List
Castaldo, A., Giordano, A., Incalzi, R.A., and Lusignani, M. (2020). Risk factors associated with accidental falls among Italian nursing home residents: a longitudinal study (FRAILS). Geriatric nursing, 41 (2), pp. 75-80. Web.
Croneri (2022). Hydration in care homes (Scotland) policy. Croner. Web.
Edmonds, C.J., Foglia, E., Booth, P., Fu, C.H.Y. and Gardner, M. (2021). Dehydration in older people: A systematic review of the effects of dehydration on health outcomes, healthcare costs and cognitive performance. Archives of Gerontology and Geriatrics, 95, pp.104-118. Web.
El-Sharkawy, A.M., Devonald, M.A.J., Humes, D.J., Sahota, O. and Lobo, D.N. (2020). Hyperosmolar dehydration: A predictor of kidney injury and outcome in hospitalised older adults. Clinical Nutrition, 39 (8), pp. 2593–2599. Web.
Grill, P., Marwick, C., De Souza, N., Burton, J.K., Hughes, C., and Guthrie, B. (2020). The burden of psychotropic and anticholinergic medicines use in care homes: Population-based analysis in 147 care homes. Age and Ageing, 50 (1), pp. 183–189. Web.
Gulka, H.J., Patel, V., Arora, T., McArthur, C., and Iaboni, A. (2020). Efficacy and generalizability of falls prevention interventions in nursing homes: A systematic review and meta-analysis. Journal of the American Medical Directors Association, 21 (8). Web.
Hamrick, I., Norton, D., Birstler, J., Chen, G., Cruz, L., and Hanrahan, L. (2020). Association between dehydration and Falls. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 4 (3), pp. 259–265. Web.
Kavouras, S.A. (2019). Hydration, dehydration, underhydration, optimal hydration: Are we barking up the wrong tree? European Journal of Nutrition, 58 (2), pp. 471–473. Web.
Kim, W.-Y., Suh, Y., Ah, Y.-M., Choi, J.-Y., Kim, K., and Lee, J.-Y. (2023). Medication-related acute care admission and inappropriate polypharmacy of Nursing Home Residents. Journal of the American Medical Directors Association, 24 (2). Web.
Lacey, J., Corbett, J., Forni, L., Hooper, L., Hughes, F., Minto, G., Moss, C., Price, S., Whyte, G., Woodcock, T., Mythen, M., and Montgomery, H. (2019). A multidisciplinary consensus on dehydration: Definitions, diagnostic methods and clinical implications. Annals of Medicine, 51 (3–4), pp. 232–251. Web.
Lee, S.W.H., Mak, V.S.L. and Tang, Y.W. (2019). Pharmacist services in nursing homes: a systematic review and meta‐analysis. British Journal of Clinical Pharmacology, 85 (12), pp. 2668-2688. Web.
Li, Y., Cen, X., Cai, X. and Temkin-Greener, H. (2019). Perceived patient safety culture in nursing homes associated with “Nursing Home Compare” performance indicators. Medical care, 57 (8), p. 641. Web.
Liu, J.Y., Reijnierse, E.M., Van Ancum, J.M., Verlaan, S., Meskers, C.G., and Maier, A.B. (2019). Acute inflammation is associated with lower muscle strength, muscle mass and functional dependency in male hospitalized older patients. PLoS One, 14 (4), pp. 215-219. Web.
Llorens-Gámez, M., Salesa, B., and Serrano-Aroca, Á. (2020). Physical and biological properties of alginate/carbon nanofibers hydrogel films. International Journal of biological macromolecules, 151, pp. 499-507. Web.
Nagae, M., Umegaki, H., Onishi, J., Huang, C.H., Yamada, Y., Watanabe, K., Komiya, H., and Kuzuya, M. (2020). Chronic dehydration in nursing home residents. Nutrients, 12 (11), pp. 35-62. Web.
O’Kane, M., Parretti, H.M., Pinkney, J., Welbourn, R., Hughes, C.A., Mok, J., Walker, N., Thomas, D., Devin, J., Coulman, K.D., and Pinnock, G. (2020). British Obesity and Metabolic Surgery Society Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obesity Reviews, 21 (11), pp. 130-187. Web.
NHS England (2022). Driver Diagrams Online Library of Quality, Service Improvement and Redesign Tools NHS England and NHS Improvement. Web.
Perrier, E.T., Armstrong, L.E., Bottin, J.H., Clark, W.F., Dolci, A., Guelinckx, I., Iroz, A., Kavouras, S.A., Lang, F., Lieberman, H.R., and Melander, O. (2021). Hydration for health hypothesis: a narrative review of supporting evidence. European Journal of Nutrition, 60, pp. 1167-1180. Web.
Reber, E., Gomes, F., Dähn, I.A., Vasiloglou, M.F. and Stanga, Z. (2019). Management of dehydration in patients suffering swallowing difficulties. Journal of Clinical Medicine, 8 (11), pp. 19-23. Web.
Ree, E. and Wiig, S. (2019). Employees’ perceptions of patient safety culture in Norwegian nursing homes and home care services. BMC Health Services Research, 19 (1), pp. 1-7. Web.
Reis da Silva, T.H. (2023). Falls assessment and prevention in the nursing home and community. British Journal of Community Nursing, 28 (2), pp. 68-72. Web.
Toots, A., Wiklund, R., Littbrand, H., Nordin, E., Nordström, P., Lundin-Olsson, L., Gustafson, Y., and Rosendahl, E. (2019). The effects of exercise on falls in older people with dementia living in nursing homes: a randomized controlled trial. Journal of the American Medical Directors Association, 20 (7), pp. 835-842. Web.
Volkert, D., Beck, A.M., Cederholm, T., Cereda, E., Cruz-Jentoft, A., Goisser, S., de Groot, L., Großhauser, F., Kiesswetter, E., Norman, K., and Pourhassan, M. (2019). Management of malnutrition in older patients—current approaches, evidence, and open questions. Journal of Clinical Medicine, 8 (7), pp. 99-104. Web.
Watanabe, K., Stöhr, E.J., Akiyama, K., Watanabe, S., and González‐Alonso, J. (2020). Dehydration reduces stroke volume and cardiac output during exercise because of impaired cardiac filling and venous return, not left ventricular function. Physiological reports, 8 (11), pp. 14-43. Web.

