Introduction
This proposal explores how community nurses can use education to mitigate incidences of exacerbation for older persons with chronic obstructive pulmonary disease (COPD). The proposal aims to inform the audience about various medical metrics that can be applied from a clinical perspective to mitigate the potential risk of adverse effects of COPD in older individuals. The benefits of evidence-based practices (EBPS) in nursing include keeping clinical interventions current and relevant to particular diseases (Henoch et al., 2018). Additionally, EBPs are essential because they improve nurses’ confidence and decision-making skills in medical situations (IGI Global, 2021). Therefore, it contributes to expertise in various diseases, enabling nurses to offer client-centered care to elderly patients.
Question Formation
The PICO (population, intervention, comparison, and outcome) question is helpful in this proposal because it captures all the key elements required for the subject matter (Marshall et al., 2017; Moglia, 2018). For instance, elderly patients are considered a key population factor within the framework, while the use of education by nurses is an intervention element under the framework. The outcome of this matter is a reduced exacerbation effect for patients with COPD (Miller, 2019).
The literature review aims to find what other scholars have said concerning the subject. While reviewing the literature, it becomes clear that the diagnostic considerations and contributing factors for COPD in older people are recognized. That means that other scholarly works form the foundation of evidence-based research regarding interventions in exacerbation incidents. Lastly, incorporating a literature review lends credibility and transferability factors to the proposal, ensuring that the work’s content is reliable and dependable from a clinical perspective (Nibber et al., 2017). Thus, the proposal does not revolve around personal thoughts, but rather the attention brought by external insights concerning exacerbations and elderly patients with chronic obstructive pulmonary disease.
Justification of the Question
It is essential to explore how nurses can utilize education to mitigate the severity of illnesses in patients with COPD. The reason is that there are many cases of mortality for older adults diagnosed with the disease. Most of the fatalities result from a lack of enlightenment on how adversity can be controlled from the patient’s perspective. Data from the World Health Organization (WHO) shows that COPD is the third leading killer disease in the world, with more than 3.23 million deaths witnessed globally in 2019.
Additionally, the British Lung Foundation (BLF) indicates that 1 in every five people has had a history of COPD, whereby 50% are currently undergoing medication (BLF, 2022). There are many deaths related to COPD that occur in people over 65 years, commonly categorized as the elderly (BLF, 2022). Therefore, based on WHO and BLF data, the number and diagnosis rates have been increasing, as shown in Figure 1.
Using this information from the two reputable sources can help clinicians understand the prevalence and identify ways to address the data trends. Park et al. (2019) also conducted a study to determine the mortality rate of COPD patients. According to their nationwide population-based cohort study, the literature shows that mortality rates increase robustly with age, as illustrated in Figure 2 below (Part et al., 2019). This means that the adverse effects of exacerbation lead to this outcome, and nurses need to use education to establish a remedy in the target population.


The proposed intervention of using education to mitigate excessive exacerbation incidences for patients with COPD is relevant due to the current evidence-based practices. Poot et al.’s (2021) study, which was based in the UK, shows that patient education programs benefit significantly in preventing exacerbations and hospital admissions. Patient education is an intervention that effectively prevents exacerbations and helps patients manage their illness.
The education involves self-management through exercise and regular review of any physical changes in the patient’s body. According to Kulakiewicz et al. (2021), “Information last updated by the National Institute for Health and Care Excellence (NICE) in 2016 says an estimated 3 million people have COPD in the UK, “of whom 2 million are undiagnosed.” Their report suggests that prevalence has increased with age, and many people are diagnosed after they reach 50 years old. National Health Service (NHS) data for 2021 show that 1.9% of the population in England has this disease (Kulakiewicz et al., 2021). Hence, the UK needs nurses to intervene in COPD.
Another factor is how a source can be considered relevant in the scientific context. The intervention measure reported in this proposal is evidence-based, as the Lutter et al. (2020) study found that educating patients leads to better outcomes in preventing mortality. It is important to note that most patients with this disease have a smoking history (Padilha et al., 2019; Meldrum et al., 2017). Hence, the risk factor is key to determining the foundational analysis nurses can use to educate older patients on combating the illness (Lutter et al., 2020). The literature review conducted will give approaches that can be useful in determining the course of action for educating patients on COPD.
Search Strategy
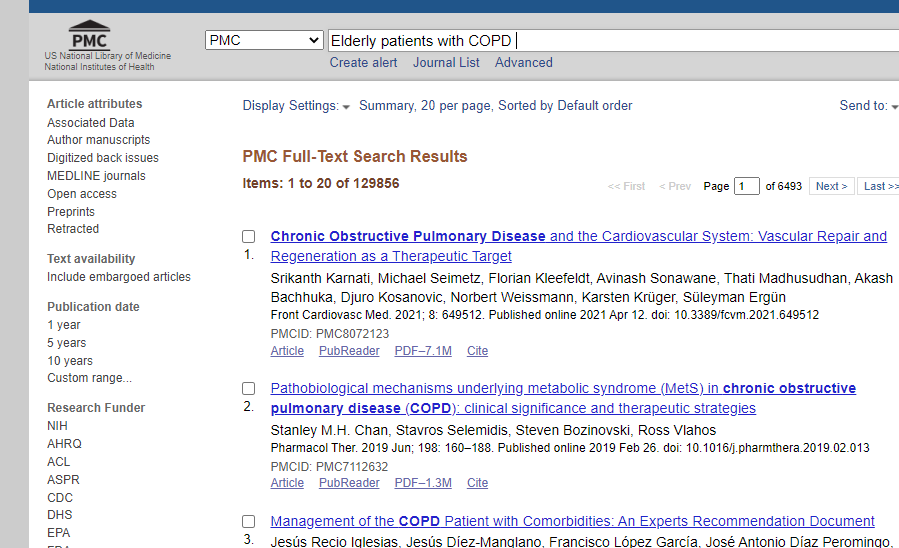
Searching for information on this proposal should be conducted from reputable sources to obtain reliable results. The National Library of Medicine (NLM) was the first database to provide access to critical data. The database through PubMed Central provides specific information related to health issues; therefore, using the tool effectively allows for the retrieval of the required information (Sadigov & Isayev, 2017). It is also essential to seek information through reputable organizations, such as the BLF and the WHO.
The research was also conducted on the BMJ website, which is a key source of quality information about safety in healthcare. Using Medline Plus also provided trusted health information for this proposal. These databases are essential since UK health agencies have approved them for research; hence, any information should be taken officially (Safari et al., 2022; Hyden & Meek, 2020). Using other sources, such as PsycINFO, would provide data that is difficult to verify and not peer-reviewed (Sandelowsky et al., 2019). Nursing is a critical field that requires scientists to include credible information to support clinical decision-making.
Some keywords were placed in the search engines for the above databases. The terms and phrases used are ‘elderly patients with COPD,’ ‘nursing interventions,’ ‘educating the public on COPD,’ and ‘nurses’ education on COPD in the UK,’ as illustrated in Table 1 below. The keywords are used simultaneously with Boolean operators such as ‘with’, ‘in’, and ‘on’. They help compose a well-structured question for the system to generate automatic results. Figure 2 illustrates that the screenshot pertains to searching for ‘elderly patients with COPD’. The process was repeated for other databases to find concrete information that guides this paper on the proposed intervention for the key population of this study.
Table 1: Keywords used in searching
Strengths and Limitations
Strengths
Getting evidence-based intervention is a process that involves various factors, where it is possible to identify weaknesses and strengths. First, the studies this proposal has used have involved qualitative and quantitative research, which means the results can be justifiable. For example, Wang et al. (2021), Cumella & Cook (2021), and Suggett et al. (2020) analysis has methodology, abstract, rationale, measurement of results, and conceptual illustrations used to create a contextual understanding.
Second, the sources used have been presented in academic and professional prose, meaning data can be attributed to the respective sources, such as citing the reference, giving the link, and explaining the thoughts. For instance, Meijer et al. (2021) have given attributes to many authors in their works, such as Burgel’s work and Wedzicha and Agusti’s research. The third strength is that the literary sources have used statistical analysis to convince readers of the points being made in their works. For example, Huang et al. (2022) used stratified probability samples in their study to give a generic risk associated with COPD patients using logistic regression factors that are key in giving a credible argument. Thus, it is essential to apply these strengths while using PICO frameworks.
Limitations
Various sources in the literature review have used various concepts that may distract from the central theme. In this case, it is difficult to comprehend one idea on COPD with elderly patients and relate it to the interventions. Hu et al. (2022) is an example of a source showing research complexity. The authors have used a practice model that combines COPD with other factors such as self-management, satisfaction, and compliance with elderly beliefs.
When reading this article, an audience may lose focus on the intervention strategy and shift to the knowledge and beliefs of the key population. The other weakness is that most of the studies were based on the general population, whereas this proposal seeks to establish intervention strategies for older patients (Wedzicha & Martinez, 2018). Therefore, it puts the research in a contentious state based on the source of information.
Conclusion
This proposal explores how nurses can leverage educational strategies to reduce the frequency of COPD flare-ups in elderly patients. This proposal uses the PICO framework since it covers all aspects required, such as intervention, population, and outcome. The subject of research is relevant since more than 3.23 million people died due to COPD in 2019 (WHO, 2022). The UK has 1.9% of its population having the disease, and nurses have been using education to patients to combat the issue (BLF, 2022).
After reading the literature review, the proposal found that educating patients on the need to control tobacco usage, exercise, and self-management is an EBP that is rampant not only in the UK but also in other parts of the world. The strengths included the literature sources’ success in conceptualizing the theme. Weaknesses include the challenge of comprehending the topic without deviating from other ideas expressed in other people’s works.
References
BLF. (2022). Lung disease in the UK. British Lung Foundation. Web.
Cumella, A., & Cook, A. (2021). S103 the provision of the five fundamentals of COPD care – findings from a UK-wide survey of people with COPD. Ease That Wheeze: Managing Risk in COPD, 2(3), 28–55. Web.
Henoch, I., Löfdahl, C.-G., & Ekberg-Jansson, A. (2018). Influences of patient education on exacerbations and hospital admissions in patients with COPD – A longitudinal national register study. European Clinical Respiratory Journal, 5(1), 67–73. Web.
Hu, W., Li, T., Cao, S., Gu, Y., & Chen, L. (2022). Influence of nurse-led health education on self-management ability, satisfaction, and compliance of elderly patients with the chronic obstructive pulmonary disease based on knowledge, belief, and practice model. Computational and Mathematical Methods in Medicine, 22(4), 1–9. Web.
Huang, Q.-M., Zhang, P.-D., Li, Z.-H., Zhou, J.-M., Liu, D., Zhang, X.-R., Zhong, W.-F., Zhang, Y.-J., Shen, D., Liang, F., Song, W.-Q., Yang, S.-G., Guan, W.-J., & Mao, C. (2022). Genetic risk and chronic obstructive pulmonary disease independently predict the risk of severe COVID-19 incidents. Annals of Thoracic Society, 19(1), 58–65. Web.
Hyden, K. F., & Meek, P. (2020). Examining the effect of adding community-based palliative care on the health-related quality of life of individuals with severe chronic obstructive pulmonary disease dissertation. The University of Colorado.
IGI Global. (2022). Research anthology on supporting healthy aging in a digital society.
Kulakiewicz, A., Macdonald, M., & Baker, C. (2021). Support for people with chronic obstructive pulmonary disease. UK Parliament. Web.
Lutter, J. I., Jörres, R. A., Welte, T., Watz, H., Waschki, B., Alter, P., Trudzinski, F. C., Ohlander, J., Behr, J., Bals, R., Studnicka, M., Holle, R., Vogelmeier, C. F., & Kahnert, K. (2020). Impact of education on COPD severity and all-cause mortality in lifetime never-smokers and longtime ex-smokers: Results of the COSYCONET cohort. International Journal of Chronic Obstructive Pulmonary Disease, 15(2), 2787–2798. Web.
Marshall, K., Knighting, K., Pilkington, M., & Kelly, C. (2017). M12 a UK survey on the experiences and views of respiratory nurses (RNs) on their role in delivering cognitive behavioral therapy (CBT) for patients with chronic obstructive pulmonary disease (COPD). Patient, Physician and Carer Perspectives, 3(3), 33–45. Web.
Meldrum, C., Martinez, C., Kloska, D., Martinez, F., Han, M. L., & Larson, J. (2017). Frailty and its components predict health-related quality-of-life in middle-aged and elderly copd people and could identify areas for age-specific interventions: An analysis of the nett study. Clinical Problems COPD, 3(6), 21–27. Web.
Miller, C. A. (2019). Nursing for wellness in older adults (6th ed.). Wolters Kluwer.
Moglia, P. (2018). Addictions, substance abuse & alcoholism (3rd ed.). Salem Press, a division of EBSCO Information Services, Inc.
Nibber, A., Chisholm, A., Soler-Cataluña, J. J., Alcazar, B., Price, D., & Miravitlles, M. (2017). Validating the concept of COPD control: A real-world cohort study from the United Kingdom. COPD: Journal of Chronic Obstructive Pulmonary Disease, 14(5), 504–512. Web.
Padilha, M., Ribeiro, A., Ramos, J., & Machado, P. (2019). Innovation in nursing education – care-COPD. Self-management promotion in people with COPD. Nurses, 11(5), 41–47. Web.
Park, S. C., Kim, D. W., Park, E. C., Shin, C. S., Rhee, C. K., Kang, Y. A., & Kim, Y. S. (2019). Mortality of patients with chronic obstructive pulmonary disease: A nationwide population-based Cohort Study. The Korean Journal of Internal Medicine, 34(6), 1272–1278. Web.
Poot, C. C., Meijer, E., Kruis, A. L., Smidt, N., Chavannes, N. H., & Honkoop, P. J. (2021). Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews, 2021(9), 3–5. Web.
Refsgaard, B., Rodkjær, L. Ø., Bregnballe, V., & Ottesen, A. L. (2018). Preventative care and home treatment in patients at risk of hospitalization due to exacerbation of COPD. Nurses, 4(8), 14–31. Web.
Roberts, P., & Priest, H. (2018). Healthcare research: A textbook for students and practitioners (4th ed.). J. Wiley.
Sadigov, A., & Isayev, I. (2017). Risk factors for readmissions in patients with COPD: How prevent the readmission rate? Chest, 152(4), 2–7. Web.
Safari, S., Carson-Chahhoud, K., Noori, M., Nejadghaderi, S. A., Sullman, M. J., Ahmadian Heris, J., Ansari, K., Mansournia, M. A., Collins, G. S., Kolahi, A.-A., & Kaufman, J. S. (2022). The burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: Results from the global burden of disease study 2019. BMJ, 4(8), 22–31. Web.
Sandelowsky, H., Krakau, I., Modin, S., Ställberg, B., & Nager, A. (2019). COPD patients need more information about self-management: A cross-sectional study in primary care. Scandinavian Journal of Primary Health Care, 37(4), 459–467. Web.
Suggett, J., Kushnarev, V., Coppolo, D., Tse, J., & Wada, K. (2020). How can the time for COPD exacerbation be delayed? A real-world study compares two oscillating positive expiratory pressure (OPEP) devices in patients with chronic obstructive pulmonary disease (COPD) or chronic bronchitis. Airway Pharmacology and Treatment, 4(6), 33–38. Web.
Wang, Z., Locantore, N., Haldar, K., Ramsheh, M. Y., Beech, A. S., Ma, W., Brown, J. R., Tal-Singer, R., Barer, M. R., Bafadhel, M., Donaldson, G. C., Wedzicha, J. A., Singh, D., Wilkinson, T. M., Miller, B. E., & Brightling, C. E. (2021). Inflammatory endotype–associated airway microbiome in chronic obstructive pulmonary disease clinical stability and exacerbations: A multicohort longitudinal analysis. Journal of Respiratory and Critical Care Medicine, 203(12), 1488–1502. Web.
Wedzicha, J. A., & Martinez, F. J. (2018). Chronic obstructive pulmonary disease exacerbations. CRC Press.
WHO. (2022). Chronic obstructive pulmonary disease (COPD). World Health Organization. Web.

