Introduction
The present paper discusses the diagnosis, case formulation, and treatment plan of a patient with a Major Depressive Disorder (MDD) with mixed features. The patient is 21 years old, Hispanic, and single. She combines studying in college and working part-time. The formulation of a cognitive case and literature on the topic of the identified diagnosis is used here to determine appropriate treatment approaches.
DSM-5 Diagnosis and NANDA Diagnosis
The patient was diagnosed with MDD with mixed features. It is noteworthy that ICD does not list MDD with mixed features, but it does include the mixed affective episode (F38.0) and various versions of mixed bipolar episodes (World Health Organization, 2016). Here, it should be pointed out that the majority of bipolar disorders, as well as depression disorders, remain the rule-out diagnoses for the described case. As established by DSM-5, both bipolar and depressive disorders can have mixed features, but the differences between them consist of which diagnostic criteria they correspond to (American Psychiatric Association, 2013). For this patient, the diagnostic criteria for depression are met, but the hypomanic symptoms do not qualify for bipolar disorder. As a result, due to the presence of hypomanic features, MDD with mixed features was diagnosed (F06.34). Thus, the DSM-5 diagnosis would be MDD with mixed features, and the rule-out medical and DSM-5 diagnoses are bipolar disorder and particular depressive and bipolar disorders.
From the perspective of NANDA, as described by Herdman and Kamitsuru (2018), two diagnoses are significant. The patient demonstrates impaired resilience as related to her depression, and evidenced by her sad affect. Furthermore, the patient is at risk of suicide related to depression, as evidenced by her recent overdose. The latter risk is denied by the patient, however. The NANDA diagnoses will help to plan the treatment for the patient and provide relevant care.
Case Formulation (Theory-Based Assessment)
The patient demonstrates multiple negative automatic thoughts that are manifested through her emotions and behaviors. Such negative assumptions can have a detrimental effect on the patient’s ability to cope with depressive symptoms (Hawley et al., 2017). She has negative reactions to events that she cannot control and things that she perceives as her failures; she views many things as personal failures. One of her apparent core beliefs is that she needs to prove her worth to people around her; she may also be operating under the assumption that she can control most aspects of her life.
Treatment Interventions with Rationale
Pharmacology
The term MDD with mixed features was introduced relatively recently. As a result, there is a limited amount of evidence on the topic, but it should be sufficient for presenting a relevant treatment plan (Rosenblat & McIntyre, 2016). The data indicate that MDD with mixed features cannot be treated like a conventional MDD (Rosenblat & McIntyre, 2016). Instead of antidepressants, the medications that have been evidenced to have an effect on MDD with mixed features are antipsychotics, including ziprasidone. According to recent studies, ziprasidone monotherapy can be described as a first-line treatment for the condition (McIntyre et al., 2017; McIntyre, Lee, & Mansur, 2016; Shim, Bahk, Woo, & Yoon, 2018). It is also the option that is relatively unlikely to be associated with metabolic changes, unlike some other recommended drugs (Rosenblat & McIntyre, 2016; Wan, Goldberg, Burdick, & Iosifescu, 2017). The patient’s BMI (26.1) indicates that she is slightly overweight, which is why metabolic considerations are important in her case. Furthermore, the patient has no cardiac issues, which is why ziprasidone’s impact on QTc is acceptable. However, it will require close monitoring in the future.
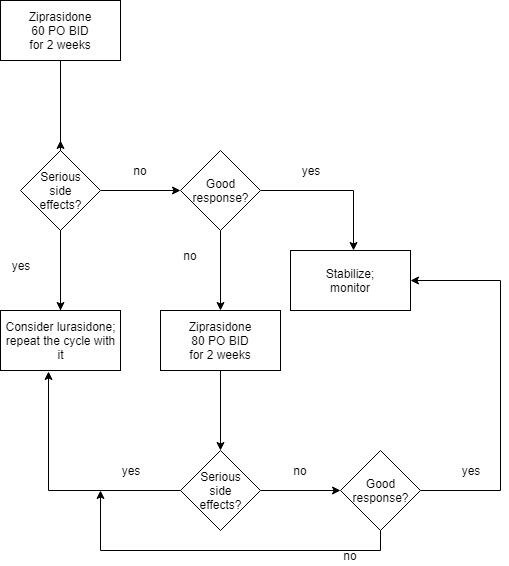
Currently, the patient takes 60 mg of Ziprasidone PO BID; the dosage has been adjusted from the initial 40 mg PO BID. Further titration is possible no sooner than in two weeks’ time, but it is not recommended to exceed 80 mg PO BID (Wan et al., 2017). Based on the relevant literature, the following algorithm should be employed for the treatment. In two weeks’ time, the patient’s response to ziprasidone should be assessed with particular attention paid to the manic and depressive symptoms and her QTc. If the response is positive, stabilization will be possible: the treatment will be continued, and adherence, as well as side effects (especially QTc), will be monitored. If major side effects become prominent, especially with respect to QTc, it is reasonable to consider another antipsychotic.
If, in two weeks’ time, the response to ziprasidone is not favorable without major side effects, the dosage should be increased to 80 mg PO BID. In two more weeks, the repeated assessment is to be carried out. If the response to this titration is not favorable, another antipsychotic should be considered. Lurasidone is the most recommended alternative; its use for MDD with mixed features was studied (McIntyre et al., 2017; Shim et al., 2018). The same titration and testing periods will be applied to lurasidone if ziprasidone does not provide the desired effects. The minimum and maximum dosages for lurasidone range from 40 to 120 mg per day (Wan et al., 2017). See Appendix A for a simple algorithm.
Diagnostic Tests/Lab Work
There are certain biological factors that can affect the mood of a person with MDD. To determine if they are present, it is necessary to measure the “thyroid function, vitamin B12, and folate levels” for the patient (Woldu, Murrough, & Iosifescu, 2017, p. 64). If the patient experiences problems with her thyroid gland or folate levels, these problems can be resolved for the improved physical and emotional state of the woman. The patient is likely to cooperate; the tests are rather standard, as pointed out by Woldu et al. (2017), which makes them accessible and feasible.
Evidence-Based Non-Pharmacologic Interventions
MDD, as well as MDD with mixed features, does not have to be treated with pharmacotherapy only. The negative core beliefs that were identified can be modified through psychotherapy (Hawley et al., 2017). Moreover, psychosocial interventions have been shown to have an impact on MDD with mixed features (Rosenblat & McIntyre, 2016; McIntyre et al., 2017; Woldu et al., 2017). One of the most well-studied approaches to MDD therapy is cognitive-behavioral therapy (CBT) (Hawley et al., 2017; Rosenblat & McIntyre, 2016). In addition, both individual and group therapy are suitable options (McIntyre et al., 2017), and they will be proposed to the patient.
The following steps will be taken to implement the intervention. The patient will be provided with general information about the methods employed during CBT, as well as individual and group therapy. Her preferences will be taken into account; based on her informed decision, the plan may be changed. With the patient’s consent, the intervention will be implemented; at least eight sessions will be required, although more would be more likely to yield positive results (Hawley et al., 2017). During the first session, the goals for the treatment will be established with the patient. Throughout the implementation, especially during the first few sessions, feedback from her will be used to determine if any changes are required.
Regarding the goals, CBT instructs patients on the behaviors and cognitive skills that can help to alleviate negative symptoms (Hawley et al., 2017). By the eighth session, the patient will aim to learn to analyze her behaviors, automatic thoughts, and core believes. Furthermore, she will learn and practice healthier coping methods, and by the end of the treatment, she will start employing them during and outside of the sessions. Thus, the therapy will aim to resolve the problems identified during the cognitive case formulation, and the achievement of these aims will be used to evaluate it.
Patient and Family Education
Aside from the information about the treatments, the patient will be coached on preventing and countering the side effects of the drugs. Given her BMI and the potential metabolic problems, she will be instructed to improve her lifestyle, especially diet and movement (Wan et al., 2017). Given that she was initially diagnosed with MDD, it is imperative to offer the patient information about MDD with mixed features. Finally, given the investment of her brother in her well-being, as well as the potential positive outcomes of family education for people with MDD (Brady, Kangas, & McGill, 2017), his involvement will also be improved through education, especially on the management of MDD.
Referrals
With the proposed plan, no referrals will be required. The psychiatric nurse practitioner working on the case would be capable of providing the services to the patient. If the patient requires significant changes to the plan, additional referrals might be needed.
Appendix A
Medication Plan
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders; DSM-5 (5th ed.). Washington, DC: American Psychiatric Publishing.
Brady, P., Kangas, M., & McGill, K. (2017). “Family matters”: A systematic review of the evidence for family psychoeducation for major depressive disorder. Journal of Marital and Family Therapy, 43(2), 245-263. Web.
Hawley, L. L., Padesky, C. A., Hollon, S. D., Mancuso, E., Laposa, J. M., Brozina, K., & Segal, Z. V. (2017). Cognitive-behavioral therapy for depression using mind over mood: CBT skill use and differential symptom alleviation. Behavior Therapy, 48(1), 29-44. Web.
Herdman, T. H., & Kamitsuru, S. (Eds.) (2018). Nursing Diagnoses: Definitions and Classification 2018-2020 (11th ed.). New York, NY: Thieme.
McIntyre, R. S., Lee, Y., & Mansur, R. B. (2016). A pragmatic approach to the diagnosis and treatment of mixed features in adults with mood disorders. CNS Spectrums, 21(S1), 25-33. Web.
McIntyre, R., Ng-Mak, D., Chuang, C., Halpern, R., Patel, P., Rajagopalan, K., & Loebel, A. (2017). Major depressive disorder with subthreshold hypomanic (mixed) features: A real-world assessment of treatment patterns and economic burden. Journal of Affective Disorders, 210, 332-337. Web.
Rosenblat, J., & McIntyre, R. (2016). Treatment recommendations for DSM-5–defined mixed features. CNS Spectrums, 22(2), 147-154. Web.
Shim, I. H., Bahk, W. M., Woo, Y. S., & Yoon, B. H. (2018). Pharmacological treatment of major depressive episodes with mixed features: A systematic review. Clinical Psychopharmacology and Neuroscience, 16(4), 376-382. Web.
Wan, L., Goldberg, J. F., Burdick, K. E., & Iosifescu, D. V. (2017). Bipolar disorders. In A. B. Simon, A. S. New & W. K. Goodman (Eds.), Psychiatry (pp. 74-87). Hoboken, NJ: John Wiley & Sons.
Woldu, H., Murrough, J. W., & Iosifescu, D. V. (2017). Depressive disorders. In A. B. Simon, A. S. New & W. K. Goodman (Eds.), Psychiatry (pp. 59-73). Hoboken, NJ: John Wiley & Sons.
World Health Organization. (2016). International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-WHO version for 2016. Chapter V. Mental and behavioural disorders (F00-F99). Web.

