Introduction
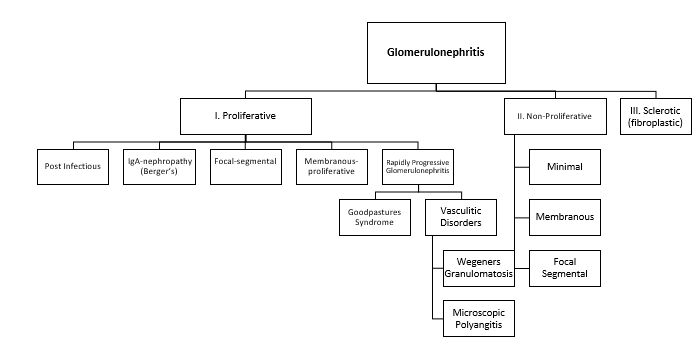
Glomerulonephritis consists of a set of renal diseases presenting as a combination of hematuria, proteinuria, edema, and hypertension. Glomerulonephritis can be caused by a variety of disorders which are caused by glomerular injury with subsequent inflammation or potential renal failure. The pathogenesis of glomerulonephritis is not well-known, but it is considered to be an autoimmune response to etiologic agents (infections) caused by genetic factors. This immunologic response triggers biological processes such as leukocyte, complement activation, and release of cytokines which trigger the inflammation or injury of the kidney (Niaudet, 2018).
Main body
There are two common types of glomerulonephritis – acute and chronic with pathophysiology differing slightly between them. In acute, the streptococcal neuraminidase modifies the host immunoglobulin G (IgG), combining with antibodies that collect in the glomeruli. Cellular proliferation occurs structurally leading to an increase in the number of cells, becoming either endocapillary or extra capillary.
Furthermore, the glomerular basement membrane thickens. In chronic glomerulonephritis, there is a reduction of the nephron mass in the injury leading to hypertrophy and hyperfiltration attempting to minimize functional nephron loss. A decline in GFR causes a rise in serum creatinine levels (Azotemia) which can lead to reductions in the production of erythropoietin, Vitamin D, as well as a reduction in excretion that may cause acidosis, hypertension, or edema (Gaut, Mueller, & Liapis, 2017).
Physical and symptom manifestations of glomerulonephritis vary on type, progression, and severity of the condition. Symptoms of acute glomerulonephritis include bloating in the face, bloody or brown urine, unusual urinating activity, and high blood pressure. Chronic glomerulonephritis commonly develops more subtly with slow-progressing symptoms such as swelling and high blood pressure, abdominal pain, nosebleeds, frequent urination, as well as an excess of protein in the urine that may lead to changes in its consistency (Ponticelli & Glassock, 2019).
Conclusion
The nephrotic syndrome appears as a primary (idiopathic) renal disease in combination with other systemic conditions. The syndrome results in non-inflammatory damage to the glomerular capillary wall. The underlying glomerular disease leads to proteinuria due to modifications in the selectivity of the glomerular capillary wall. As a result, permeability increases to plasma proteins with loss of albumin in the urine as well as proteins carrying hormones, Vitamin D, and clotting inhibitors.
Nephritic syndrome is characterized by glomerular inflammation, the degree of which impacts the severity of renal dysfunction and clinical manifestations. Immunologic perturbations which are common in glomerulopathies can be seen with either antibody binding to structural components or formation of antigen-antibody complexes that cause glomerular injury. The filtration barrier begins to malfunction resulting in inflammation and there is salt retention leading to volume expansion, hypertension, and edema (Dylewski, Kooienga, & Teitelbaum, 2018).
References
Dylewski, J., Kooienga, L., & Teitelbaum, I. (2018). Chapter 24: Nephrotic syndrome versus nephritic syndrome. In E. V. Lerma, M. H. Rosner, & M. A. Perazella (Eds.), CURRENT diagnosis & treatment: Nephrology & hypertension (2ed.) (211-216). New York, NY: McGraw Hill Education.
Gaut, J. P., Mueller, S., & Liapis, H. (2017). IgA dominant post-infectious glomerulonephritis update: pathology spectrum and disease mechanisms. Diagnostic Histopathology, 23(3), 126-132. Web.
Niaudet, P. (2018). Overview of the pathogenesis and causes of glomerulonephritis in children. Web.
Ponticelli, C., & Glassock, R. J. (2019). Treatment of primary glomerulonephritis. Oxford, England: Oxford University Press.
