Rationale
Mental health is an important aspect of one’s well-being, and treating psychological problems is a complex task that requires high-quality care. According to recent data, the rates of mental health issues increase each year, with the pandemic becoming a catalyst for people experiencing problems with depression, anxiety, addiction, and other psychological conditions (Hossain et al., 2020). The quality of addressing such concerns depends on many factors, one being patient-provider communication. For instance, community mental health centers care for a large portion of the population, offering individual and group therapy, treatment plans, and consultations (Thornicroft et al., 2016). The team communicates with service users, carers, and family members daily, discussing diagnosis, treatment, and support.
An opportunity lies in improving the quality of communication between the team and service users. In such cases, ineffective communication may lead to conflict and poor health outcomes (Kwame & Petrucka, 2021). In contrast, scholarship suggests that communication that centers on patient needs and considers their opinion in the treatment process leads to high user satisfaction and better results (Hashim, 2017). SProvider-patient interactions have to emphasize transparency, involvement, and clarity. According to Aggarwal et al. (2016), professionals’ resistance to the involvement of service users is a major issue in modern mental health care. Thus, a chance arises to improve communication through a change project.
As mentioned above, the inclusion of service users in their care is a significant part of treatment that is currently not being sufficiently met in healthcare overall. Furthermore, it is also not being addressed in the chosen community mental health center. The proposed project considers a strategy for improving provider-patient communication and increasing shared decision-making through changes in communication. Therefore, it addresses the need for better communication between the team of professionals and service users, their families, and loved ones.
While laws do not strictly dictate patient inclusion in decision-making, the focus on patient-centered care is a pillar of current organization regulations. The Institute of Medicine considers the patient-centered approach inseparable from high-quality care (Agency for Healthcare Research and Quality [AHRQ], 2022; Greenhalgh et al., 2018). Moreover, research demonstrates that involving the service user in the decision-making process is beneficial for the organizational status and low risks of malpractice or patient complaints (Birkeland et al., 2021 ). The patient’s perspective on their own treatment is necessary to comply with the recommendations of major international healthcare organizations.
The problem of provider-patient communication is connected to the domain of patient-centered care. As the AHRQ (2022) outlines, healthcare professionals must ensure that their services respect patients’ needs. Based on the value of autonomy, the mental health team must encourage patient participation and consider the preferences of one’s carers and loved ones (Howick et al., 2018). Communication plays a significant role in improving patient participation, as it facilitates feedback and knowledge-sharing. Without effectively interacting with the patient, one cannot gather important information and see the patient’s perspective of their mental well-being.
Objectives
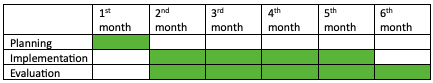
Considering the information about the selected problem, the project should aim to develop and implement a program that improves communication and shared decision-making in a community mental health center. The project involves a process intervention, and the specific SMART goal is to improve service user satisfaction ratings with their participation in the healthcare process in the next six months. As the issue of communication affects patient outcomes, focusing on patient feedback is vital for ensuring that the change project has benefits. The presented goal adheres to the SMART framework:
- Specific – the aspect of patient engagement is the central one in improving communication.
- Measurable – Patient feedback will be used to measure the outcomes.
- Achievable – The mental health center wishes to improve patient-provider communication and has resources for change.
- Realistic – Patient-centered care is an essential part of communication improvement.
- Time-Scaled – The plan is designed to be implemented in 6 months.
The potential benefits are summarized in the SWOT analysis in Appendix A. However, due to the variety of dimensions that can be affected by the project, a detailed description is presented below. First, the intervention focuses on advantages for the service users. According to Howick et al. (2018), positive and effective communication increases patient engagement, allowing patients to voice their opinions and participate in treatment planning. Moreover, shared decision-making improves treatment initiation and continuation, meaning individuals are less likely to discontinue visiting the medical facility (Vermeir et al., 2015). Therefore, in the mental health center, where continuous care is vital for patients, effective communication can benefit care quality and patient outcomes.
In physical health research, the clinical advantages of effective communication and patient involvement are connected to health improvement. In particular, pain reduction and improvement of symptoms and condition severity may follow the treatment that focuses on patient needs (Naslund et al., 2016). Similarly, mental health benefits include better symptom management, increased medication adherence rates, and other patient outcomes (Howick et al., 2018). The clinical benefits affect long-term patient health as well.
For the organization, improved communication and increased patient satisfaction result in a better clinic status. Thus, it may also see more opportunities for expansion or other change programs. Staff may also benefit from improved communication and experience greater satisfaction with their work, deliver better care, and grow as professionals.
Moreover, the organization that has better patient care and sees improvements in patient satisfaction, better adherence rates, and more are also likely to have better financial outcomes due to fewer complaints and legal issues. As noted above, the dimension of quality addressed by this project is patient-centered care. Therefore, benefits for the quality of care are apparent – the facility will introduce measures that emphasize patient voices, advocating for their inclusion in care.
Context
The project involves a single mental health community center. The local context is a large city with a vast population diversity. Thus, patient communication must be considerate and well thought-out to support the service users’ unique features. Furthermore, as it is a mental health community organization, individuals who come to the center have expectations about their care and may possess stigma or reservations about mental health care. The view of mental health may impact the project, and communication should overcome this barrier if it arises.
The problem for this project arose from the common issues that mental health facilities and healthcare organizations have. The lack of patient engagement continues to be an issue in medical care, and mental health is no exception (Hashim, 2017). At the same time, scholarship highlights the need to include service users in their care and encourage active participation (Howick et al., 2018). This result can be achieved by training providers – the mental health team – to involve patients through communication. The issue in the selected mental facility and the vital role of communication in improving service user outcomes drove this project.
Intervention
The intervention is focused on improving patient-provider communication. In particular, it aims to involve service users, families, and carers in the process of care and help them voice their opinions about their health and treatment. Thus, the proposed change is to educate the mental health team to include five areas of focus when talking to service users – feelings, ideas, concerns, impact, and expectations (Hashim, 2017). Thus, each provider has to include questions from every area when talking to the service user or their family and use this feedback in treatment planning.
Each area of focus has several questions on which practitioners can base their communication. The first part – feelings – covers service users’ worries and concerns. Here, the mental health care team members should inquire about patients’ emotions and make sure that their comments are taken into consideration. Such questions as “What is worrying you the most?” and “How do you feel about that?” can increase the understanding of patient needs (Hashim, 2017).
The second area of question is ideas – service user feedback is vital to planning and decision-making. One may ask the patient, “In your opinion, what caused…?” to investigate their suspicions and learn more about their lives (Hashim, 2017). This type of examination may also uncover new information.
The third type of question is related to patient concerns and fears. For instance, the provider may inquire, “Are you worried something might happen?” and “What concerns you about …?” in regard to the service user’s health (Hashim, 2017). These questions reveal some negative opinions and anxieties patients have and allow them to express what they are thinking. The fourth type of inquiry deals with impact – such questions as, “What difficulties do you face because of …?” focus on specific issues and help one create a better plan for the patient (Hashim, 2017).
Finally, the last area of focus is expectations – service users should be allowed to say what they want to achieve through medical help. Here, one may ask, “What would you like to get out of this visit?” and “What can I do for you?” to highlight the role of the patient in this discussion (Hashim, 2017). The combination of these questions involves the patient in every step of the treatment process.
Implementation Plan
The intervention based on the questions outlined above will take the form of a short 2-hour training with follow-up check-ins and patient surveys (Appendix B). First, the project leader will select a team of professionals to participate in the intervention. Then, a survey will be designed to inquire about service users’ satisfaction with their involvement in health care and patient-provider communication quality. Team members will also answer similar questions to measure their views on patient engagement. The survey will then be administered to the patients to collect data before intervention. Following that, the mental health team will go through training that talks about the aforementioned questions and their value to patient health.
Several months after the education has been provided, the project leader will keep in contact with the team and examine their use of the new approach. Finally, at the end of the project, surveys will be distributed among patients and providers again to collect information for comparison. Based on both data sets, conclusions will be made to see how the communication has improved and what future steps can be taken. During the project, the leader will employ the coaching leadership style and focus on training the mental health care team based on their current knowledge and strengths. Moreover, the communication plan will include opportunities for feedback and encourage open conversation.
Team Structure and Roles
The project requires the community center’s mental health team to participate. However, the project leader is the main actor who distributes educational materials and communicates with the team to collect feedback and evaluate their performance. Team members’ responsibilities do not change significantly – they are asked to include an additional set of questions into their routine. Therefore, the process requires minimal changes to the work operations and does not impact the team specifics or relationships in any way.
The key stakeholders involved in this project are the team, service users and their families, and the community center. All stakeholders have a high interest in the success of this project, which means that the project leader has to communicate the goals and the results to them. The center also has high power as it supports the intervention and provides resources. It is vital to comply with the organization’s values when implementing the project. Service users and employees are stakeholders with low power, but they can provide feedback about the quality of the intervention, which may affect its development. Frequent meetings with the team will be held to allow service providers to voice their opinions and share their ideas.
Risk Management
As outlined in Appendix A, several risks may endanger the effectiveness of the project. First, service users may not be engaged in the new changes. As a result, they may not participate in surveys, which will result in no information for project monitoring. Furthermore, they may not talk to staff members, showing how the change is not favorable for their involvement. The center may overcome this risk by explaining the value of engaging with the project to patients through printed materials. Staff members may also quickly describe the project at the beginning of each meeting to raise awareness.
The next potential risk is provider resistance to the project. Employees may view the intervention negatively and not use the new questions during patient visits. This issue may strongly affect project outcomes and decrease care quality. It is vital to start the training by discussing project benefits and keeping in contact with team members to encourage their participation. Finally, the last risk arises as new questions may prolong patient visits, decreasing center efficiency. Team members can overcome this problem by prioritizing questions that are the most relevant to the service user’s current concerns.
Evaluation Plan
As noted above, the evaluation plan will include service user and team surveys that investigate their satisfaction with patient involvement. The choice of a quantitative approach in the project will yield data that can demonstrate intervention effectiveness. The data will be collected before and after the implementation for comparison, and the surveys will be checked for quality of evidence to ensure that the results are consistent and reliable.
References
Agency for Healthcare Research and Quality. (2022). Six domains of healthcare quality. Web.
Aggarwal, N. K., Pieh, M. C., Dixon, L., Guarnaccia, P., Alegria, M., & Lewis-Fernandez, R. (2016). Clinician descriptions of communication strategies to improve treatment engagement by racial/ethnic minorities in mental health services: A systematic review. Patient Education and Counseling, 99(2), 198-209. Web.
Birkeland, S., Bismark, M., Barry, M. J., & Möller, S. (2021). Does greater patient involvement in healthcare decision-making affect malpractice complaints? A large case vignette survey. Plos One, 16(7). Web.
Greenhalgh, J., Gooding, K., Gibbons, E., Dalkin, S., Wright, J., Valderas, J., & Black, N. (2018). How do patient reported outcome measures (PROMs) support clinician-patient communication and patient care? A realist synthesis. Journal of Patient-Reported Outcomes, 2(1), 1-28. Web.
Hashim, M. (2017). Patient-centered communication: Basic skills. American Family Physician, 95(1), 29-34.
Hossain, M. M., Tasnim, S., Sultana, A., Faizah, F., Mazumder, H., Zou, L., McKyer, E., Ahmed, H., & Ma, P. (2020). Epidemiology of mental health problems in COVID-19: A review. F1000Research, 9(636), 1-16. Web.
Howick, J., Moscrop, A., Mebius, A., Fanshawe, T. R., Lewith, G., Bishop, F. L., Mistiaen, P., Roberts, N., Dieninyte, E., Hu. X-Y., Aveyard, P., & Onakpoya, I. J. (2018). Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. Journal of the Royal Society of Medicine, 111(7), 240-252. Web.
Kwame, A., & Petrucka, P. M. (2021). A literature-based study of patient-centered care and communication in nurse-patient interactions: Barriers, facilitators, and the way forward. BMC Nursing, 20(1), 1-10. Web.
Naslund, J. A., Aschbrenner, K. A., Marsch, L. A., & Bartels, S. J. (2016). The future of mental health care: Peer-to-peer support and social media. Epidemiology and Psychiatric Sciences, 25(2), 113-122. Web.
Thornicroft, G., Deb, T., & Henderson, C. (2016). Community mental health care worldwide: Current status and further developments. World Psychiatry, 15(3), 276-286. Web.
Vermeir, P., Vandijck, D., Degroote, S., Peleman, R., Verhaeghe, R., Mortier, E., Hallaert, G., Van Daele, S., Buylaert, W., & Vogelaers, D. (2015). Communication in healthcare: A narrative review of the literature and practical recommendations. International Journal of Clinical Practice, 69(11), 1257-1267. Web.
Appendices
Appendix A – SWOT Analysis
Appendix B – Gantt Chart