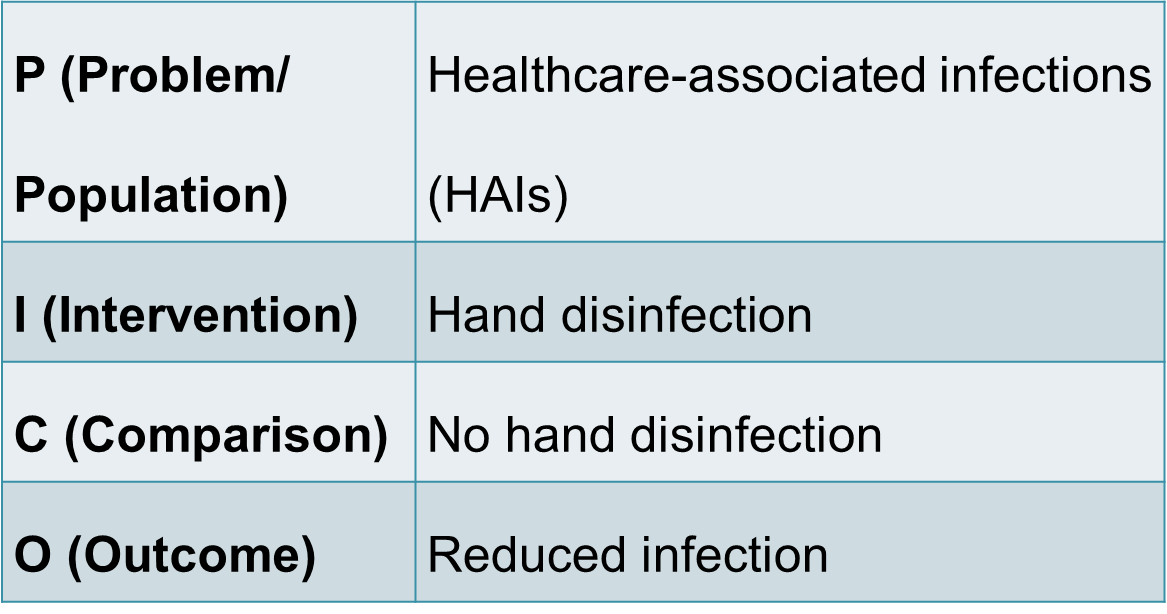
PICO formula
Evaluating the effect of hand disinfection among healthcare workers on nosocomial infections is crucial to develop a strategy to decrease the spread of infection. Using the PICO formula, the clinical question was developed: does hand disinfection among healthcare workers reduce healthcare-associated infections (HAIs) compared with no hand disinfection? The following slides present recent research findings on the issue of hand hygiene and hospital-acquired infection.
Quality of Healthcare
Safety and effectiveness constitute two integral parts of quality healthcare. Hence it is crucial to conduct research aiming to resolve issues associated with healthcare provision and improve its quality and safety. Healthcare providers implement a patient-centered approach, and the main responsibility for its efficiency lies with healthcare staff. In this regard, infection control and prevention of healthcare-associated infection spreads is critical to ensure patients’ safety.
Healthcare-Associated Infections (HAIs)
Healthcare-associated infections (HAIs) refer to infections patients can get while receiving healthcare. Any healthcare facility poses a risk for its patience to catch an infection due to invasive devices and procedures implementation. According to McLaws (2015), the most common HAIs are central line-associated bloodstream infections, catheter-associated urinary tract infections, ventilator-associated pneumonia, and surgical site infections. Apart from the obvious risks for patients’ safety and healthcare quality, HAIs are associated with additional costs and prolonged hospital stays.
Hand Hygiene for Infection Control in Hospitals
Therefore, it is critical to reduce nosocomial infections to improve healthcare quality and lower the risks for patients receiving treatment in hospitals. Improved hand hygiene is widely believed to contribute to HAIs prevention (McLaws, 2015). Hand washing and hand antisepsis are considered the simple and efficient measure, listed by the WHO in its guidelines on hand hygiene (Tyagi et al., 2018). The issue remains especially acute for low- and middle-income countries, where hygiene norms are followed less frequently.
Research Evidence of Hand Hygiene Benefits
Hand hygiene is an essential procedure that prevents bacteria from spreading from the patient’s environment to the patient. As indicated by research, adequate hand hygiene improves clinical service, helps avoid prolonged hospital stays, and lowers infection risks for patients with weakened immune systems (McLaws, 2015). Besides, according to Tyagi et al. (2018), hand disinfection is critical for newborn care, helping prevent sepsis. Complications and lethal outcomes resulting from HAIs can also be avoided. Therefore, healthcare workers providing service must ensure to reduce the spread of germs.
A Downside of Hand Hygiene Practices Among Healthcare Workers
Work-related dermatitis resulting from focusing on hand-hygiene constitutes an additional risk for healthcare workers. Besides, the lack of a reasonable approach to the issue indicates safety risks in developing countries. Vinodhini and Devi (2016) state that insufficient awareness of the problem and lack of implemented hand hygiene practices can also reduce healthcare quality. Therefore, despite high effectiveness, solely hand hygiene cannot be considered a sufficient measure to reduce HAIs in hospitals.
Risk Factors Contributing to HAIs rates
Despite the indisputable benefits of hand hygiene among healthcare workers, one should realize the additional risk factors contributing to the HAIs rates. As McLaws (2015) reports, “older age, immunosuppression, admission to the intensive care unit, longer length of stay, and indwelling devices” pose additional risks for healthcare quality (para. 1). The risk of medical device contamination also partly depends on hand hygiene.
Alternative Infection Control Practices Among Healthcare Workers
Along with hand disinfection, there are various measures implemented for infection control in healthcare facilities. In particular, medical staff’s personal protective equipment, the safe use and disposal of sharps, reprocessing of reusable medical equipment and instruments, and routine environmental cleanings are crucial to control and prevent infection. Besides, respiratory hygiene is important to avoid bacteria spread in hospitals.
The Effects of No Hand Disinfection
Poor practice in hand hygiene among healthcare workers can result in adverse outcomes of patients’ health. In particular, decreased occupational safety of employees, the additional risk of invasive techniques for patients, the transmission of drug-resistant bacteria are associated with inadequate hand disinfection by medical staff. In developing countries, the lack of hand hygiene is especially harmful as it contributes to the risks associated with insufficient healthcare quality (Chadwick, 2019). As a long-lasting effect, decreased patients’ trust in the healthcare facility worsens the problem.
The Comparison of Hand Hygiene and No Hand Disinfection
It is crucial to draw parallels addressing the clinical question of whether hand disinfection among healthcare workers reduces HAIs compared with no hand disinfection. When improved hand hygiene is always considered a beneficial factor for HAIs reduction in hospitals (Vinodhini & Devi, 2016), lack of hand hygiene proves to be an always detrimental factor (McLaws, 2015). At the same time, a healthcare facility needs to implement various policies aimed at infection control since hand hygiene constitutes only one of the risks for medical workers and patients. Drawing attention to the importance of hand disinfection is crucial to raise awareness and improve healthcare quality.
Recommended Practices to Improve Hand Hygiene
To ensure patients’ safety, it is crucial to develop and adhere to practices that proved to be effective in infection control. For instance, as Vinodhini and Devi (2016) suggest, infection control committees need to monitor the situation and take steps to reduce HAIs. Developing education programs for healthcare workers and displaying guidelines on improving hand hygiene is also necessary to remind of its importance. Besides, medical waste management and the immunization of medical workers at risk are also crucial to improving hand hygiene.
Findings and Conclusion
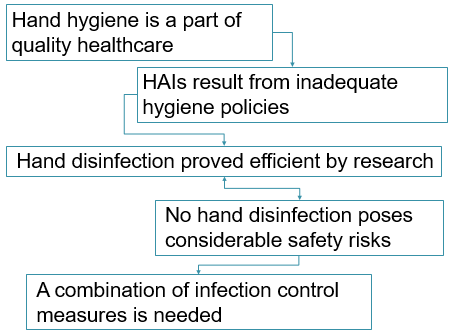
To sum up, recent research has shown that hand hygiene and sufficient hand disinfection is a critical part of providing safe and quality healthcare in hospitals and medical facilities. The increased rates of HAIs indicate the need to implement measures aimed to lower bacteria spreads, and medical workers’ hand hygiene remains the critical factor. Even though additional steps need to be taken, hand disinfection among healthcare workers reduces HAIs compared with no hand disinfection.
References
Chadwick, C. (2019). Infection control 4: Good hand-hygiene practice for hospital patients. Nursing Times, 115(9), 27-29. Web.
McLaws, M. L. (2015). The relationship between hand hygiene and health care-associated infection: It’s complicated. Infection and Drug Resistance, 8, 7-18. Web.
Tyagi, M., Hanson, C., Schellenberg, J., Chamarty, S., & Singh, S. (2018). Hand hygiene in hospitals: An observational study in hospitals from two southern states of India. BMC public health, 18(1), 1299. Web.
Vinodhini, K., & Devi, B. A. (2016). Study on infection control practices among health care workers in a speciality hospital, Chennai. Pollution Research, 35(3), 549-555. Web.

