Abstract
African Americans use hospice services at far lower rates than other groups and are more likely to experience untreated pain at the end of their lives. The objective of the present systematic review was to synthesize the evidence of barriers to hospice care utilization that African Americans are experiencing.
A systematic literature search was conducted using PubMed, CINAHL, PsycINFO, and Web of Science databases (from 2009 to 2019) in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Research articles that examined barriers to hospice care utilization for African Americans were included in this review. Fineout-Overholt’s Level of Evidence was used for quality appraisal. A total of eight studies were synthesized in this review. Barriers to hospice care utilization were categorized into
- lack of knowledge and awareness;
- barriers in the health care system;
- privacy concerns;
- fear and anxiety;
- lack of communication;
- racism, discrimination, or stigma;
- cultural values, spiritual and religious perspectives.
Findings revealed that several obstacles to effective hospice care can be observed, ranging from personal to cultural and systemic elements. The factors in this review provide guidance on scholarly and practical implications on the topic and proposing future policy to increase health participation of racial and ethnic minorities.
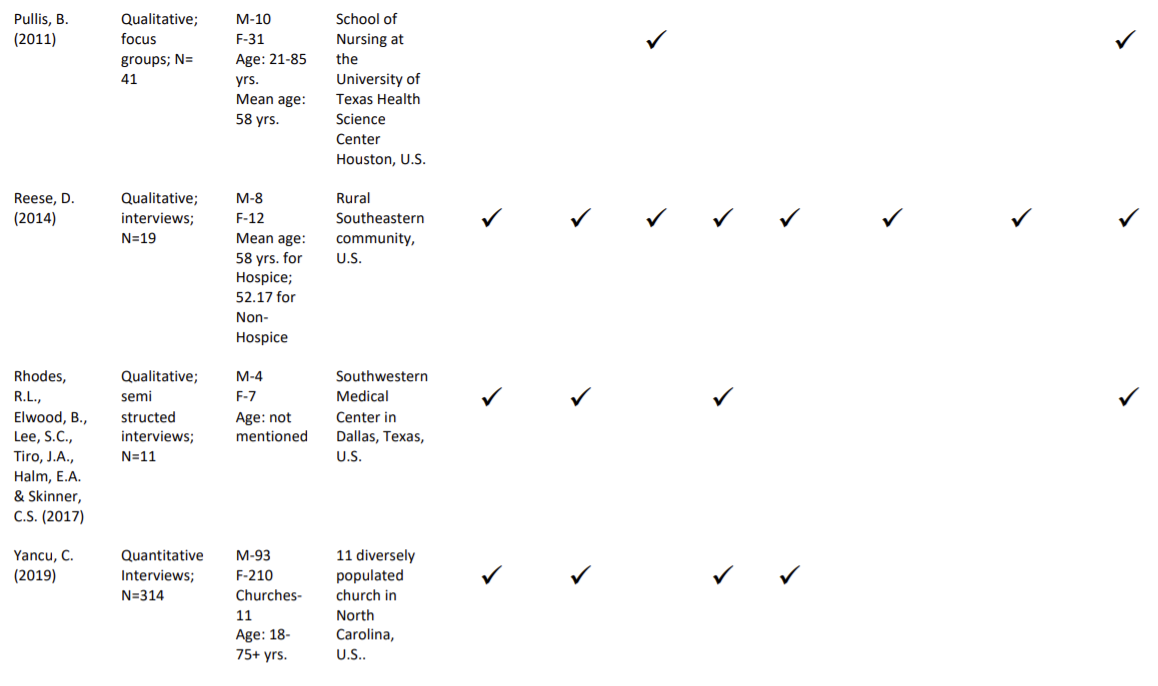
End-of-life care typically provided by hospice care is critical to vulnerable populations due to the benefits it provides when assisting patients with severe illnesses in specialized facilities. The African American community is disproportionately affected in the population utilizing hospice care within the framework of end-of-life medicine. According to the statistical data provided by the National Hospice and Palliative Care Organization (NHPCO) (2019), 1.55 million Medicare beneficiaries received hospice services and only 8.2% of those hospice patients were African American as seen in Figure 1 below.
Compared to other races, African Americans are typically lower in hospice use when compared to the ethnic breakdown of the national population, where they represent 13.4%. End-of-life care is critical to vulnerable populations due to the benefits it provides when assisting patients with severe illnesses in specialized facilities. The abundance of barriers and the lack of progress in addressing them within the hospice health care system urge an in-depth study of the full range of obstacles that prevent African Americans from using hospice care.
Barriers
The existing scholarly literature on the topic of barriers to hospice use by African Americans is broad and includes both qualitative and quantitative studies (Johnson et al., 2016; Rhodes et al., 2017; Stevens, 2016). However, while there are several systematic reviews investigating the topic of barriers, Washington systematic review addressed the issue with particular concern with faith and spirituality (Washington et al., 2008).
Washington et al.’s systematic review (2008) has addressed faith among many other barriers that do not allow African Americans to use the services of hospice care facilities. This research was aimed at the general identification of barriers, including socioeconomic, hospice philosophy’s conflict with culture or personal values, lack of knowledge about such services, lack of trust to facilities, and others.
However, no particular attention was paid to the manifestations of faith and religious or spiritual attitudes, beliefs, and practices that are commonly followed by the African American communities and obstruct their willingness or opportunities to enjoy the benefits of hospice care. Unlike Washington et al. (2008), the current systematic review is not focused on faith and religious values as the most under-investigated but very important barrier.
Aim
The current systematic review is aimed at presenting a new perspective on the issue of barriers to end-of-life care provided to the African American community by broadening the spectrum of perceived barriers. The scarcity of an up-to-date systematic review that would synthesize the relevant barriers to hospice care for African Americans imposes the need to concentrate on recent studies. The review is expected to broaden the understanding of health disparities burdened on African Americans, the most influential barriers to their access to hospice care and will provide a basis for adequate intervention development.
The novelty of the proposed research is twofold and is validated by the need to fill the literature gap on the topic of the common barriers to hospice utilization among African Americans. Firstly, the gap that has been identified in research entails the lack of recent publications of hospice utilization obstacles for the African American community.
Most of the systematic reviews on the topic were published more than ten years ago, and only a few of those research studies are conducted using a qualitative review method. Secondly, as the review of similar research by Washington et al. (2008) shows, the general overview of barriers is provided. However, faith is considered one of the influential factors that define the utilization of end-of-life care in the African American community.
Methods
Research team
Our research team consists of four social welfare doctoral students at the University of Hawaii at Mānoa. The common thread that binds this team of researchers is they are all MSW and are grounded in a broad spectrum of disciplines and methodological traditions designed to enhance and promote the well-being of individuals, families, and the larger community-in-need. All four researchers are currently students in a Systematic Review Course at the time of this writing.
One of the researchers is a native of Tonga, raised in Hawaii has had hospice experience and the opportunity to intern at St. Francis Hospice Bereavement Services; is currently a medical social worker working directly with patients and hospice providers in the referral process. A second researcher is a native of Norway, is a 4th year PhD student in Social Welfare and has had extensive hospice experience.
The third researcher, a second year PhD student, was born and raised in Hawaii and has had intense personal hospice experience, also with the St. Francis Bereavement Services. The fourth researcher, also a second year PhD student in Social Welfare; was born and raised in Dominican Republic, working with the indigenous population at the Hospice Service Center.
Search strategy
While in discussion on racial disparities in health care, our research team decided to focus on the barriers and challenges of African Americans and hospice care. Here is the full list of search terms related to African Americans, hospice and barriers that each of the four researchers input used to search titles and abstracts for journal articles and dissertations between the years 2009 and 2019 in the following databases: PsychINFO, PubMed, Web of Science, and CINAHL.
((“African American” OR “African-American” OR “Black Americans” OR Black* OR “Afro Latino” OR “Afro-Latino” OR “Afrolatino”) AND (Hospice) AND (questionnaire* OR survey* OR interview* OR “focus group*” OR “case stud*” OR “observational stud*”) AND (utili*ation OR usage OR use OR access) AND (barrier* OR obstacle* OR hindrance* OR challenge* OR deterrent*) AND (qualitative or “mixed method*” OR quantitative))
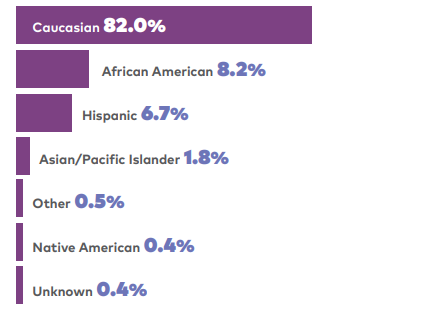
Using the full list (as described in the above paragraph) to load each database search, Figure 1. illustrates the yield per database.
Figure 2. Search Results per Database.
After removing duplicates, this search produced 1,544 results. (illustrated in Figure 2. PRISMA). Two teams of two authors (Team A and Team B) reviewed the abstracts and introductions (772 articles per team) to determine whether they met the eight criteria. Each researcher worked with two entries: EXCLUDE or INCLUDE.
Within each team, each person independently reviewed the 772 articles (abstracts and introductions); the individual respective columns were copied and pasted adjacent to their teammate’s selections onto one sheet to compare results in a third column. Within each team, the two authors reviewed and discussed each article that differed between them. The end results per team were: Team A = 37 and Team B = 20, totalling to 57 articles.
At this point, the two teams discussed streamlining the research by possibly doing two separate submissions for publication and re-reviewed the 57 articles, looking specifically at research design and scanning full text. These articles were then exchanged between the two teams for further and objective review which yielded the following: Team A = 17 and Team B = 10. A total of 27. We decided at this point to do one review with mixed methods.
Screening and Data Extraction
The research team carried out searches in databases PsycINFO, PubMED, Web of Science, and CINAHL with the journals’ impact factors ranging between 1.226 and 4.18. Acceptable articles were written in the last ten years between 2009 and 2019. Eight criteria were used to determine exclusion of an article in this study. The researchers utilized the following exclusion criteria:
- It was a duplicate.
- Not about African American
- Not about hospice.
- It was a Systematic Review.
- It was not empirical.
- It was not in the U.S.
- It was not a dissertation or article.
- Not in English.
The full text of these articles (27) was then reviewed by each of the four researchers by applying additional criteria in order to yield the most robust data. a) Was the study framed or grounded in hospice practice? and/or b) Did the study use primarily African American samples? Once the additional criteria were applied, a total of 8 articles met one or both criteria for inclusion in this study. As seen in the PRISMA flowchart in Figure 2, the search resulted in locating eight most relevant articles on the subject matter.
Results
All eight of our articles were focused on our population of interest which is African Americans in the U.S. The articles were able to report data which sufficiently answered our research question about barriers to hospice utilization for African Americans. Methodology in the studies varied. Five of the studies were qualitative, two quantitative and one mixed methods research.
Purposive, convenience, and random sampling were used in the studies, with the majority using purposive sampling. Sample size in the studies varied between 10-314 respondents, with the majority being female and adults ages 50 and above. Terminally ill patients, caregivers, family members, physicians, hospice and non-hospice participants were used in the various studies depending on the aim. Interviews, focus groups, and surveys were used to elicit the data. Only African American participants were included in the research. The topics of these papers can be divided into several categories:
- lack of knowledge and awareness;
- barriers in the health care system;
- privacy concerns;
- fear and anxiety;
- lack of communication;
- racism, discrimination, or stigma;
- cultural values, spiritual and religious perspectives.
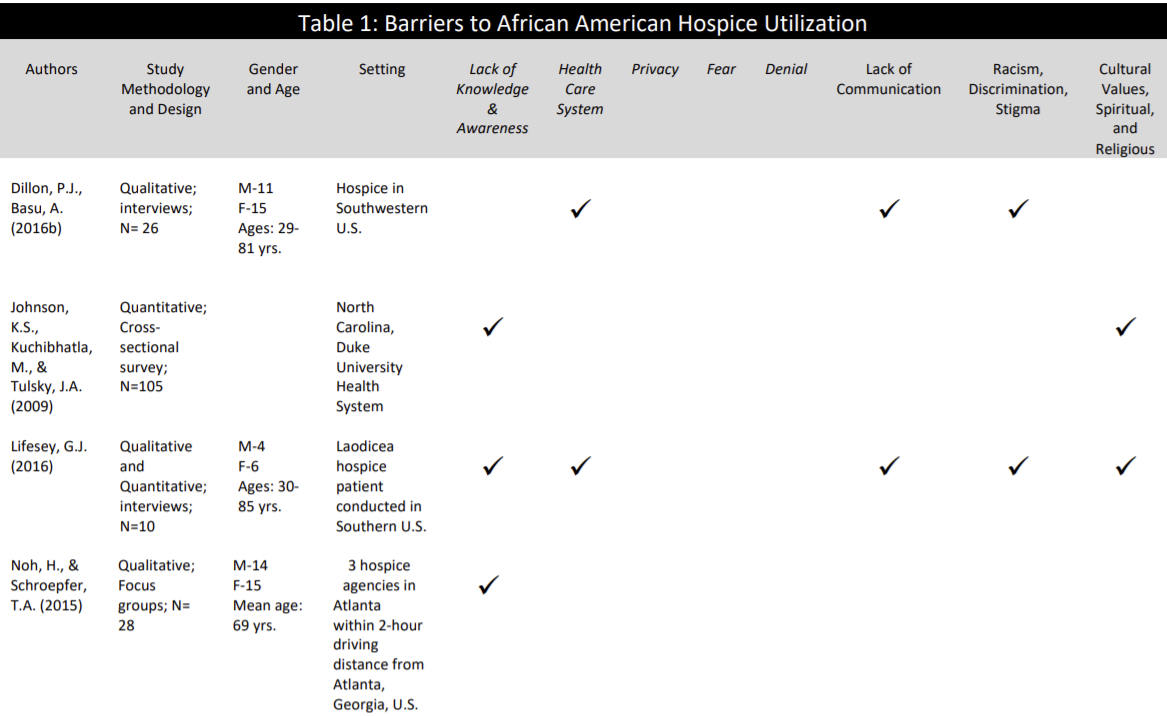
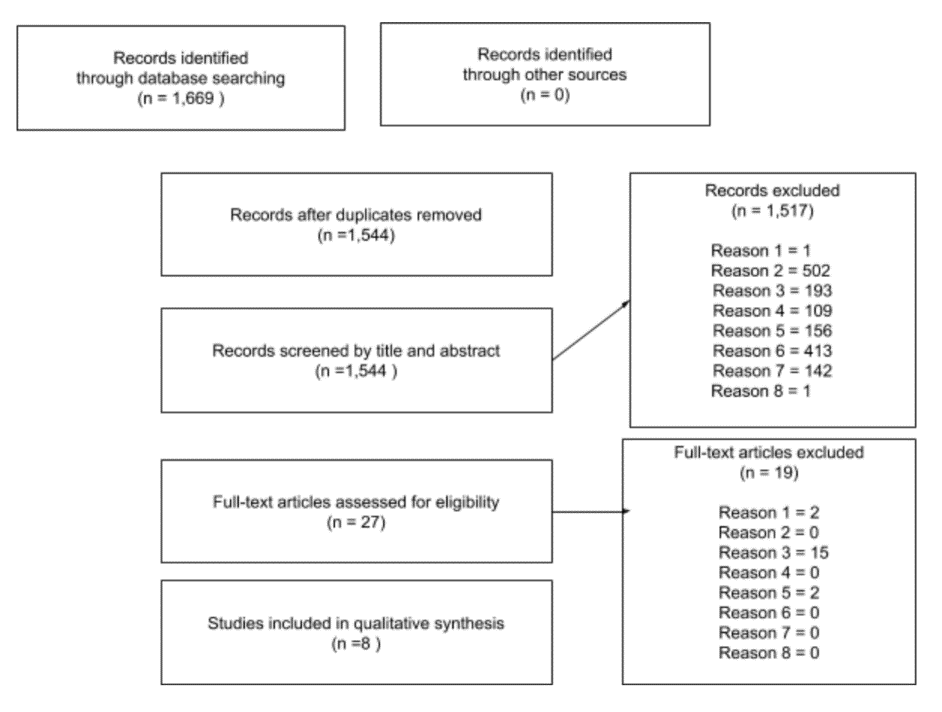
The eight selected articles are summarized in Table 1 (Appendix A).
Lack of Knowledge and Awareness of Hospice Services
Almost all of the studies reviewed emphasized the lack of understanding, awareness, exposure, philosophies, and services of hospice care (Johnson, Kuchinhatla, & Tulsky, 2009; Lifesey, 2016; Noh, & Schroepfer, 2015; Reese, D. 2004; Rhodes., Elwood, B., Lee, Tiro, , Halm, & Skinner, 2017; Yancu, 2019).
A study of terminally ill patients reported that they lacked knowledge about hospice services. (Noh & Schroepfer, 2015). “We was totally against it because you know, we didn’t really understood, didn’t have the knowledge of what they [hospice care] was really about…”, said one patient (Noh & Schroepfer, 2015, p. 291).
Similar findings were reported from the other studies. Exploring hospice participation and barriers for African American’s, Yancu’s study (2019) reported that the preference to provide care at home was a barrier. This is a clear manifestation of the lack of knowledge and awareness of hospice services. A hospice provider shared experiences with working with African Americans and explained that African Americans have minimum information about hospice (Rhodes et al., 2017, p. 6).
Also, Reese (2014), reported that the lack of knowledge of hospice philosophy was a barrier for hospice utilization. Johnson and colleagues (2009) found that among 105 African American respondents in their study, 19% of them reported that hospice was unheard of. Furthermore, the lack of exposure to hospice significantly influenced the desire for African American’s to enroll in hospice services compared to whites (Johnson et al, 2009).
Health Care System
Four of eight studies found that the healthcare system was a barrier to African American’s utilization of hospice. A hospice provider reported that mistrust of the healthcare system has multiple occurrences in medical literature as a result of their knowledge of historical events. Mistrust in the healthcare system in medical literature because they believed this knowledge impacted their access to adequate care (Rhodes et al., 2017). Similarly, participants in Reese’s study reported experiences of negative health care experiences such as inadequate care, limited access to services, and lack of insurance.
Three of the eight studies indicated that there are barriers to accessing hospice care due to inconsistencies in the healthcare system (Dillon, et al, 2016; Lifesey, 2016; Reese, 2014). Respondents reported that the history of the lack of services has led to inadequate care, access to services and quality of care. Furthermore, the lack of diversity in hospice staff, African American hospice staff and the unwillingness to participate in government programs were also mentioned barriers (Reese, D. 2014; Yancu, C., 2019).
Privacy
Hospice care entails close involvement and interactions with hospice staff and not everyone is comfortable with this kind of relationship. Respondents in Reese’s study (2014) reported that a barrier to hospice utilization is the need for privacy. Some felt that hospice care in the home was an intrusion (Pullis, 2011)
Fear
Fear was a theme among a few of the studies. Some respondents expressed that they had a fear of strangers, a fear of being harmed by hospice staff, and some simply felt intimidated. Others feared that excessive use of medications or that denial of food and water would kill them (Resse, 2014). The fear of death and losing a loved one was also mentioned (Rhodes et al, 2017). Some respondents relayed a reluctance to plan for death and that hospice meant that they were giving up hope (Yancu, 2019).
Denial
Two of eight studies reported a barrier to hospice enrollment was due to feelings of denial (Reese, 2014; Yancu, 2019). In both studies respondents shared that there was denial in the terminality of the diagnosis.
Lack of Communication
Inconsistencies in communications and misinformation is another barrier faced by African Americans. Participants felt that there was a major lack in communication by healthcare professionals (Dillon & Basu, 2016; Lifesey, 2016; Reese, 2014) In two studies, participants mentioned that they were being mistreated (Dillon & Basu, 2016; Lifesey, 2016).
Reese (2014) revealed that some were ignored, and others not being informed of terminal prognosis. Another study mentioned that they received wrong information from family, friends, and through media that were misleading. As a result, hesitation set in when hospice services were offered (Noh, H., & Schoepfer, 2015).
Racism, Discrimination, and Stigma
In two studies, respondents reported experiences of discrimination and stigma (Dillon, 2016; Lifesey, 2016). Reese’s study (2014) reported racism as a contribution to a lack of referrals and communication from health providers.
Cultural Values, Spiritual, and Religious Beliefs
Several studies attributed cultural, spiritual, and religious beliefs as being a barrier to hospice use among African Americans (Johnson et al., 2009; Reese, 2014) ; Rhodes et al., 2017. A minister shared how some may feel that hospice meant they’ve lost faith in God felt that hospice meant that they have lost hope. The discussion of death is taboo and the responsibility to “care for own” are examples of cultural values that influence decisions of hospice enrollment. The lack of involvement in one own’s care and disrespect of personal values and beliefs by white professionals also were reported (Reese, 2014).
Discussion
Hospice care services play a major role in the management of patients with life limiting illness. Evidence suggests that hospice services are underutilized among African Americans compared to other ethnic groups. Therefore, a systematic review of empirical studies examining the barriers to hospice care utilization among African Americans was critical. Among the 8 studies identified in this review, six studies were qualitative, two studies were quantitative, and one was mixed methods.
Even though the importance and recommendations for hospice care has gained momentum in the past few years, the evidence on an increased hospice care utilization among African Americans with life limiting illness still seems to be lacking. Barriers, such as lack of knowledge, the fear of death, fear of inadequate treatment that will hasten the end of life, and contradiction between religious beliefs and palliative care perception obstruct African American’s access to hospice care (Rhodes et al., 2017).
While our results do not indicate spirituality as the main barrier, the literature suggests that faith might be one of the key barriers that are under-addressed due to the lack of culturally sensitive care in hospices. The religious and spiritual aspect that contributes to African Americans’ diminished access to hospice care is addressed via focus groups and semi-structured interviews (Johnson et al., 2016; Rhodes et al., 2017).
Presently, several obstacles to effective hospice care can be observed. These include the general lack of awareness about their significance stemming from mistrust toward the healthcare system, in general. The specified concerns are linked to the presence of deeply seated fears, including the fear of strangers leading to the mistrust for healthcare experts.
Likewise, the unwillingness to plan for death among patients since the specified process is perceived as morbid in its nature adds to the list of complications in delivering care to local residents. The specified attitudes typically entail the denial of death itself, preventing patients from evaluating their options objectively. Furthermore, the presence of cultural barriers and problems of communication obstruct the process of delivering care to the target demographic.
However, personal factors reducing the possibility of establishing proper care also have a tangible effect. For instance, the perception of home care as intrusion into one’s personal space, as well as the associated fears, and the cultural standards that encourage the target population to opt for in-home care, shape the access to relevant services for vulnerable groups (Rhodes et al., 2017). Additionally, issues such as the absence of crucial resources needed for providing decent-level care stand in the way of improving public health in the target area. In order to examine the issue in its full extent and discover key socioeconomic and sociocultural underpinnings of the problem.
Nonetheless, there is a gap in the primary investigation of faith as a barrier to hospice care access. Therefore, the current project fills the gap in addressing faith and spiritual beliefs as the barrier to hospice utilization by African Americans by means of a qualitative review approach.
References
Dillon, P. J., & Basu, A. (2016b). Toward eliminating hospice enrollment disparities among African Americans: A qualitative study. Journal of Health Care for the Poor and Underserved, 27(1), 219–237. Web.
Johnson, K. S., Kuchibhatla, M., & Tulsky, J. A. (2009). Racial differences in self-reported exposure to information about hospice care. Journal of Palliative Medicine, 12(10), 921–927. Web.
Lifsey, G. J. (2016). Hospice and African Americans: Exploring barriers to effective end-of-life care. [Doctoral Dissertation, Capella University]. ProQuest Dissertations Publishing. Web.
National Hospice and Pallative Care Organization. (2020). NGPCO facts and figures. Web.
Noh, H., & Schroepfer, T. A. (2015). Terminally ill African American elders’ access to and use of hospice care. American Journal of Hospice & Palliative Medicine, 32(3), 286–297. Web.
Pullis, B. (2011). Perceptions of hospice care among African Americans. Journal of Hospice & Palliative Nursing, 13(5), 281–287. Web.
Reese, Dona J., Smith, M. R., Butler, C., Shrestha, S., & Erwin, D. O. (2014). African American client satisfaction with hospice: A comparison of primary caregiver experiences within and outside of hospice. American Journal of Hospice & Palliative Medicine, 31(5), 495–502. Web.
Rhodes, R. L., Elwood, B., Lee, S. C., Tiro, J. A., Halm, E. A., & Skinner, C. S. (2017). The desires of their hearts: The multidisciplinary perspectives of African Americans on end-of-life care in the African American community. American Journal of Hospice & Palliative Medicine, 34(6), 510–517. Web.
Yancu, C. N., Farmer, D. F., & Leahman, D. (2010). Barriers to hospice use and palliative care services use by African American adults. American Journal of Hospice & Palliative Medicine, 27(4), 248–253. Web.
Appendix A