Introduction
Alzheimer’s disease, similarly known as senile dementia of the Alzheimer’s type, is a chronic, deteriorating brain condition that significantly impacts memory, cognition, and self-care abilities. Patients with Alzheimer’s (AD) experience neurodegeneration and memory loss, total mental deterioration, and early death. The cure for this condition is yet to be determined. The appearance of senile plaques, silver-positive neurofibrillary tangles (NFT), and pronounced cortical neuron loss are significant signs of AD. Even though, during the previous years, a substantial quantity of specific knowledge has accumulated, the reasons for these advances are still not fully understood. To consider and understand them deeply, Alzheimer’s disease should be discussed from different perspectives, such as its causes and recent studies conducted about the treatment.
History of Alzheimer’s Disease and Studies for Treatment
Three phases can be identified in the history of the Alzheimer’s disease (AD). In the first, Alzheimer and Kraepelin established the pathological and clinical foundations of the illness. Then there is the present period, which began in the late 1970s and has concentrated on the biological origins of dementia (Fletcher et al. 1). In between, there comes the time dementia was understood in terms of psychodynamics, which is virtually entirely disregarded in most AD histories. Most people credit Alois Alzheimer and Emil Kraepelin with creating the contemporary notion of AD. Alzheimer described the pathological features of AD after the study of a 51-year-old woman who experienced increasing dementia, focal symptoms, hallucinations, and delusions. Her post-mortem brain was discovered to have multiple senile plaques and a newly discovered disease formation called neurofibrillary tangles.
Age-related dementias presented psychiatrists with two different issues in the 1930s. According to a large autopsy series published in 1933, there is a fragile association between dementia symptoms and the existence of post-mortem brain disease (Berger et al. 810). In other cases, the senile plaques and neurofibrillary tangles discovered in the brains of dementia patients were also found in the brains of patients who had never before displayed any symptoms of dementia (Fletcher et al. 2). American psychiatrists working under the direction of David Rothschild at the Worcester State Hospital created a novel theory of dementia in the middle of the 1930s that addressed both sets of issues.
Nonetheless, age-associated dementia is more than simply the normal, inevitable brain aging or sickness that leads to cognitive loss. Dementia results from a dialectical interplay between the brain and the aged person’s sociocultural surroundings (Berger et al. 803). When it came to understanding dementia, it was believed that the chemical mechanisms in the brain that led to plaques and tangles were at least as crucial as pre-morbid personality traits, emotional stress, disruptions of familial support, and social isolation. Ageism was coined by Robert Butler in 1968 to describe the process of systematic stereotyping and discrimination against people because they are elderly, much as racism and sexism do with skin color and gender.
In Butler’s opinion, one of the worst aspects of the conventional view of aging was the idea that physical and mental degradation was inevitable as people aged. Butler and other gerontologists argued that sickness processes rather than aging were better understood as the source of the physical and mental loss often attributed to old age. In this view, “senility” was used to designate anyone beyond sixty who was experiencing a problem rather than a medical diagnosis.
Recent Studies for the Treatment of Alzheimer’s Disease
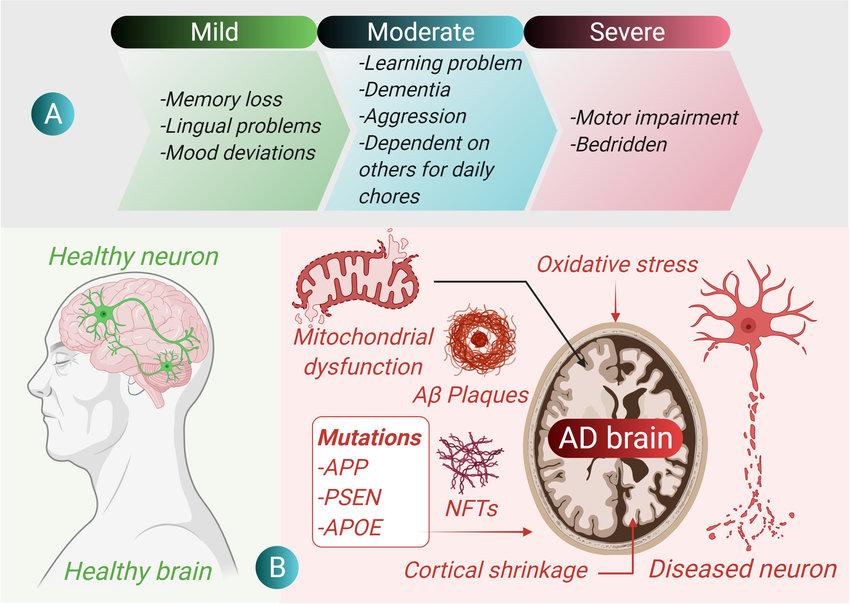
The picture presented above demonstrates three types of Alzheimer’s Disease. Based on the studies for treatment, Lecanemab, a different Alzheimer’s drug, has demonstrated potential in treating mild Alzheimer’s disease and moderate cognitive impairment brought on by Alzheimer’s disease. It could be accessible in 2023; therefore, according to a phase 3 clinical trial, the drug significantly reduced the rate of cognitive loss in individuals with early Alzheimer’s disease by 27% (Huang et al. 12). Lecanemab functions by inhibiting the aggregation of amyloid plaques in the brain. The greatest trial examined whether removing amyloid plaque clusters from the brain may delay the condition’s onset (Huang et al. 10). The Food and Drug Administration (FDA) is investigating Lecanemab as another research examines the medication’s potential efficacy for those at risk of developing the disease, such as those who have a first-degree family (a parent or sibling) who has the condition (Huang et al. 10). Another monoclonal antibody with potential is Donanemab. Phase 3 of the trial for the medication has begun.
A vast rise in research aimed at finding medications to prevent the illness has resulted from the ongoing growth in life expectancy, which has led to a rapidly expanding number of individuals with AD. Despite all scientific efforts, there are currently no potent pharmacotherapeutic interventions. The only known treatments are symptomatic and aim to balance the disease’s neurotransmitter imbalance. Nonetheless, agitation and anger were found to be the most often reported behavioral crises in a 2018 study that examined the variables linked to behavioral crises related to dementia (Backhouse et al. 100). Therefore, Brexpiprazole is a partial agonist of the dopamine receptor D2 and is used as an adjuvant treatment for schizophrenia and major depressive disorder (Backhouse et al. 103). It is now the subject of phase III clinical studies for treating agitation in patients with moderate to severe AD. Compared to a placebo, topline results from these studies, which were released in 2017, showed a decrease in agitation symptoms (Backhouse et al. 100). However, complete trial results have not yet been published.
Dronabinol, a CB1/CB2 partial agonist, is now being tested in Phase II studies as an additional medication for managing severe agitation in AD patients. The anxiolytic properties of tetrahydrocannabinol (THC) are well established. Additionally, nabilone is presently being examined in a small-scale phase III clinical study to determine whether it may lessen agitation in AD patients. The sponsors have requested a more extensive survey following the presentation of encouraging preliminary results at the annual Alzheimer’s Association International Conference.
Solanezumab is another medication that could be more efficient if administered earlier in the disease. A monoclonal antibody, it failed to show any effect for people with mild or severe Alzheimer’s disease (Lee et al. 9). Recent tests indicated that the medication appeared safe, and solanezumab is still being assessed in the preclinical stage of the illness (Lee et al. 9). Avoiding devastation Saracatinib, a medication once created as a potential cancer therapy is currently being studied for Alzheimer’s disease (Lee et al. 9). The medication reversed some memory loss in rats by turning off a protein that enabled synapses to function again (Lee et al. 6). Saracatinib is now undergoing human trials as a potential therapy for Alzheimer’s.
Causes of Alzheimer’s Disease
Aging
Age-related changes in the brain’s weight and volume, the growth of the ventricles, and the loss of synapses and dendrites in particular brain regions affect cognitive function. The pathological characteristics of AD, such as SP and NFT, accompany these alterations. There are two different aging processes at play in AD. A myelin breakdown brought on by age and the loss of locus caeruleus (LC) cells causes microglia to produce less Ab, and terminal varicosities supply noradrenaline to the cortex (Luckey et al. 520). Tau-immunoreactive NFT initially appears early in the LC in aging, moderate impaired cognitive (MC), and AD, perhaps generating continuity. The blood-brain barrier may deteriorate with age due to cell death in the LC. This implies that vascular factors could contribute to Alzheimer’s Disease.
Deterioration of Anatomical Pathways
The Cholinergic Pathway
One of the initial hypotheses for the origin of AD was a particular degradation of the cholinergic neurotransmitter system. At first, studies showed that the disease was associated with noticeable losses of acetylcholine in the brain (Breijyeh and Karaman). Later, researchers conducted a decrease in choline acetyltransferase (CAT) in the cerebral cortex region and a reduction in acetylcholinesterase (ACHE), especially at a later phase of the Alzheimer’s disease.
Cortico-cortical Pathways
The effect of the disease on the patients’ cerebral cortex is another issue that should be researched. In many incidences the line of evidence always shows the anatomical connections between various regions of the cerebral cortex may deteriorate in AD (Zhao et al.). The local neuronal circuit repeated and represented by columns or modules is a crucial aspect of the cerebral cortex’s architectural structure. Depending on the location, the diameter of each cortical module ranges from 500 to 1000 mm (Zhao et al. 9). There are particular connections between ordered groups of columns.
Infectious Agents-Based Theories
Infectious agents have been reported to cause Alzheimer’s disease. These agents include viruses that may activate microglia and pericytes, leading to amyloid deposition. In AD, antibodies to the herpes simplex (HSV) virus may be found in the cerebral spinal fluid (CSF). HSV can cause aberrant protein production, leading to PHF and NFT. Therefore, the BBB has restricted the therapeutic efficacy of many inhibitors, antibodies, and other methods.
Theories Based on a Malfunction in the Mitochondria
First, enlarged and deformed mitochondria are present, with a decrease in cerebral metabolic rate, which is an early sign of AD. Second, it’s possible that some of the enzymes needed to use carbohydrates, particularly mitochondrial indicators like phosphofructokinase (PFK) and pyruvate dehydrogenase, are deficient in AD (Bayliak et al.). Third, excess maternal versus paternal inheritance may contribute to the familial aggregation of AD in a way that is compatible with mitochondrial inheritance. In response to the possibility that mitochondrial dysfunction in AD may have a hereditary foundation, the mitochondrial cascade hypothesis (MCH), which maintains that mitochondrial failure is the primary cause of the events leading to the ACH, was created. Fourth, an adapter protein evolutionarily conserved signaling intermediate in the Toll pathway (ECST) may act as a molecular sensor to track cell homeostasis in response to oxidative damage by Ab (Bayliak et al.). Failure might result in severe mitochondrial injury, apoptosis, synaptic dysfunction, and neuronal death. In response, protective molecules might be precisely activated.
Head Trauma
The activation of microglia and immune cells in the central nervous system causes the first injury from head trauma to frequently spread to initially unaffected regions via inflammatory cytokines, aggravating the initial damage. In addition, investigation shows there is evidence of head trauma with AD (Lee et al. 9). Amyloid precursor protein (APP) is seen in neuronal perikarya and the DN surrounding Ab deposits in survivors of head injuries, much like in AD (Lee et al. 10). Ab is converted from APP inside the synaptic terminal fold of axons; glia is unnecessary for this process. Thus, the creation of APP may be a component of the brain’s response to neuronal injury. Later studies showed that patients with head traumas had more APP-i immunoreactive neurons in these areas.
The specific neurons in the medial temporal lobe emitted significant quantities of APP. The discovery that APP and the precursor to epidermal growth factor exhibit structural similarities support the hypothesis that APP may have neurotrophic properties. Additionally, bNFT could influence how injured neurons respond (Lee et al. 8). These findings suggest that the production of pathogenic proteins due to brain damage is one method by which AD illness starts and is subsequently propagated within the brain by cell-to-cell transfer.
Diet and Malnutrition
Author Alan initially suggested that starvation can contribute to Alzheimer’s disease. Clinical findings of AD patients, who typically exhibit emaciation and cachexia, uTIs, terminal bronchopneumonia, and low triceps skinfold, provide weight to this notion. Low cerebral glucose and oxygen metabolism, as well as insufficient tryptophan, folate, iron, and vitamin B12 levels, may also be present in low serum albumin levels (Al Mansoori et al. 1383). These symptoms suggest that AD suffers from a protein-calorie malnutrition condition, which may trigger the development of NFT due to persistent calcium and magnesium nutritional deficiency. Establishing cause and effect is difficult with this kind of hypothesis since malnutrition can be a side effect of the sickness caused by the patient’s mental state.
Genetics-based Theories
APP
A variety of Ab peptides are produced when the secretase cleaves APP. Ab42 is the most common of these peptides and is mainly found in isolated Ab deposits. Ab40, which is more soluble and is present in conjunction with blood vessels, on the other hand, may show up later on in the course of the illness. APP mutations in the Ab coding area may cause Ab38 to deposit in vessel walls, especially in severe cerebral amyloid angiopathy cases. Early soluble peptide oligomers, which differ depending on the type of mutant, may also be responsible for the cause of AD. This would provide a genetic explanation for the differences in pathogenesis between FAD cases.
Additionally, the Amyloid Cascade Hypothesis (ACH), the most significant explanation of the molecular pathophysiology of AD, was developed in response to the discovery of Ab. The ACH states that the deposition of Ab peptides is the primary pathogenic event in AD, leading to the production of SP and NFT, cell death, and dementia. Throughout this process, SP and NFT also pick up additional proteins, including Apo E, ubiquitin, and complement.
PSEN Genes
The endoplasmic reticulum membrane has nine trans-membrane domains that comprise the entire length of PSEN. PSEN is broken down by end proteolysis, assembled into the g-secretase complex, and then transported to the cell surface, potentially affecting how the APP is processed. Therefore, mutant PSEN1 could facilitate normal APP cleavage by 42-specific-g-secretase, increasing the deposition of amyloid-forming species. PSEN could also cause g-secretase activity to decline through loss of function. The PSEN1 gene may be crucial for cell differentiation because it participates in notch signaling (Al Mansoori et al. 1383). PSEN1/2 genes may also be involved through interactions with the transcriptional coactivator cAMP-response element binding (CREB-binding) protein, which is essential for controlling gene expression or through the disruption of cellular calcium homeostasis Ephrin-B may also exert neuroprotective effects through PSEN1, and a loss in this protection may contribute to AD.
Treatment of Alzheimer’s Disease
Three cholinesterase inhibitors (Cis) have been approved to treat mild to moderate AD. For moderate-to-severe AD, memantine is an additional therapy option. Antipsychotics and antidepressants are used in conjunction to treat the disease’s behavioral symptoms. Potential therapies include substances that address the pathological causes of the illness, such as extracellular amyloid (A) plaques and intracellular neurofibrillary tangles (NFTs)
Anti-cholinesterase Drugs
The cholinergic hypothesis of AD states that cholinergic systems in the basal forebrain are damaged early in the disease process. This results in memory loss and deterioration of other cognitive and noncognitive functions, such as neuropsychiatric symptoms. It has been proposed that CIs can enhance cholinergic transmission by delaying the breakdown of acetylcholine between synaptic clefts. Galantamine, donepezil, and rivastigmine are the three CIs that are currently approved as the most effective treatment for mild to moderate AD.
Antagonist of N-Methyl-D-Aspartate
An additional treatment option for moderate-to-severe AD is memantine. This drug is supposed to protect neurons against excitotoxicity. According to RCT trials, those with moderate to severe AD showed improved cognition, ADL, and behavior after six months of use (Gavrilova et al. 2777). Another comprehensive evaluation that included six RCT trials concluded that memantine might decrease the behavioral and psychological signs and symptoms of dementia. Memantine studies’ most reported adverse effects were disorientation, headaches, dizziness, and agitation.
Combining Therapies
The combination of memantine and donepezil showed a substantial advantage over the placebo group regarding cognitive function, language, ADL, behavioral, and general state on parallel groups of patients with moderate to severe AD. However, this advantage was not observed in those with mild to powerful AD. CIs and memantine may affect behavioral symptoms. However, if BPSD progresses, these antidementia drugs could not be as effective as required, requiring the administration of additional medications.
Serotonin reuptake inhibitors (SSRIs), including fluoxetine, sertraline, paroxetine, citalopram, and fluvoxamine, are commonly recognized as some of the most effective antidepressants for treating comorbid depression in AD dementia. Anxiety and agitation are treated with benzodiazepines, but they can also irritate older adults more. In general, AD patients and older persons, higher benzodiazepine usage has been associated with a quicker decrease in cognitive and functional abilities. Carbamazepine and similar anticonvulsant drugs can also somewhat reduce BPSD in AD.
Diagnosis
Therefore, using specialized biomarkers, it is now possible to distinguish between dementia brought on by various illnesses and Alzheimer’s disease. The recommendations use biomarkers such as brain imaging of amyloid plaques, changes in brain volume, and measures of tau and amyloid in spinal fluid to diagnose dementia brought on by Alzheimer’s disease, in addition to preclinical Alzheimer’s and moderate cognitive impairment (MCI) brought on by Alzheimer’s.
Care of Patients with Alzheimer’s Disease
With the introduction of new medical therapies, professionals must ensure that medication is adequately supervised at home and keep an eye out for any adverse side effects. It is also essential to maintain the safety of patients both at home and while driving. Unsafe driving can predispose to Alzheimer’s disease. Therefore, patients with this condition should take appropriate precautions during driving.
Develop good communication skills. Limit interruptions, make eye contact, and address the patient directly. It is important to ask patients who have hearing loss to wear a hearing aid. Simplify phrases by presenting just one idea or instruction at a time. Keep an eye on your tone of voice; patients often react more to your style than your content. Use nonverbal clues like pointing, pantomiming, or nodding in place of words when necessary. Avoid discussing the patient in front of them, as speech production may be preserved more effectively than comprehension.
Maintain the patient’s hygiene by practicing routine bathing, especially early in the morning when the patient is at rest. Reduce options for dressing or arrange the patient’s pre-selected clothing. Try to obtain duplicates of similar styles if the person insists on wearing the same outfits daily so that beloved clothing can be washed. When finished, some patients experience vulnerability. Throughout the course of Alzheimer’s, maintaining an appropriate diet and hydration is crucial in in-patient care, but it can become an even more significant issue as the illness progresses. Numerous symptoms, such as depression, visuospatial alterations, agnosia that make it challenging to recognize foods, reductions in olfactory and taste sensitivity, poor judgment, forgetfulness, agitation, and dysphasia, can have an impact on nutrition.
Conclusion
The primary cause of dementia, AD, continues to have several unusual risk factors and diseases connected to it. It is incredible how far research has come to understand the disease process and create treatments for AD. For a deeper understanding of the underlying processes, an integrative examination of AD diagnostic pathways that differ between individuals affected by various causatives is necessary. The development of advanced approaches for the early diagnosis as well as the identification of the most effective targets for therapy is made possible by the identification of AD biomarkers and other observable pathological mechanisms.
Works Cited
Al Mansoori et al. “The effects of bariatric surgery on vitamin B status and mental health.” Nutrients 13.4 (2021): 1383.
Backhouse et al. “What do we know about behavioral crises in dementia? A systematic review.” Journal of Alzheimer’s Disease 62.1 (2018): 99-113.
Bayliak et al. “High fat high fructose diet induces mild oxidative stress and reorganizes intermediary metabolism in male mouse liver: Alpha-ketoglutarate effects.” Biochimica et Biophysica Acta (BBA)-General Subjects 1866.12 (2022): 130226. Web.
Berger, Thomas, et al. “Adult hippocampal neurogenesis in major depressive disorder and Alzheimer’s disease.” Trends in Molecular Medicine 26.9 (2020): 803-818. Web.
Breijyeh, Zeinab, and Rafik Karaman. “Comprehensive Review on Alzheimer’s Disease: Causes and Treatment.” Molecules, vol. 25, no. 24, 2020, p. 5789.
Faiyaz et al. “Nanomaterials in Alzheimer’s disease treatment: a comprehensive review.” Frontiers in Bioscience-Landmark 26.10 (2021): 851-865. Web.
Fletcher et al. “The neuropsychiatric biopolitics of dementia and its ethnicity problem.” The Sociological Review, vol. 70, no. 5, SAGE Publications, 2021, pp. 1005–24.
Gavrilova, Svetlana I., and Anton Alvarez. “Cerebrolysin in the therapy of mild cognitive impairment and dementia due to Alzheimer’s disease: 30 years of clinical use.” Medicinal Research Reviews 41.5 (2021): 2775-2803. Web.
Huang et al. “Clinical trials of new drugs for Alzheimer disease.” Journal of biomedical science 27.1 (2020): 1-13. Web.
Lee, J.H., Yang, D.S., Goulbourne, C.N., Im, E., Stavrides, P., Pensalfini, A., Chan, H., Bouchet-Marquis, C., Bleiwas, C., Berg, M.J. and Huo, C. “Faulty autolysosome acidification in Alzheimer’s disease mouse models induces autophagic build-up of Aβ in neurons, yielding senile plaques.” Nature Neuroscience (2022): 1-14. Web.
Luckey, A.M., Robertson, I.H., Lawlor, B., Mohan, A. and Vanneste, S. “Sex differences in locus coeruleus: a heuristic approach that may explain the increased risk of Alzheimer’s disease in females.” Journal of Alzheimer’s Disease 83.2 (2021): 505-522.
Zhao, Z., Zhu, H., Li, X., Sun, L., He, F., Chung, J.E., Liu, D.F., Frank, L., Luan, L. and Xie, C. “Ultraflexible electrode arrays for months-long high-density electrophysiological mapping of thousands of neurons in rodents.” Nature Biomedical Engineering (2022): 1-13.
