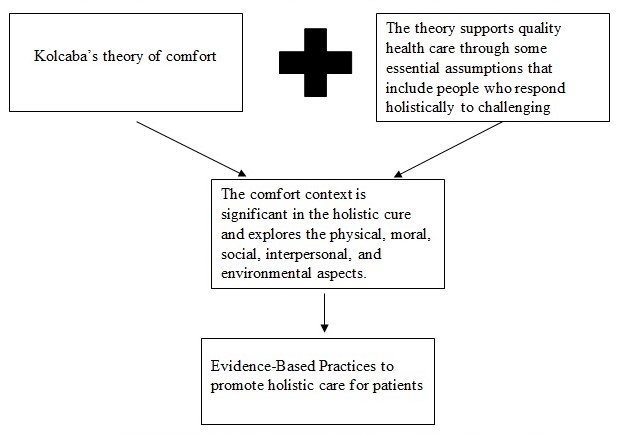
Narrative Explanation of the Visual Representation
The theory of comfort by Katharine Kolcaba describes comfort as a fundamental need for relaxation, ease, or transcendence for all people from stressful health care situations. Aksoy Derya & Pasinlioğlu (2017) argue that patient comfort occurs in three ways: relaxation, convenience, and transcendence, with the argument that consolation may improve patient, family, and nursing health care behavior. Nursing caregivers have the duty to identify patients’ and their families’ needs. These conditions are changed by intervening factors that the nurses do not influence. With these principles in mind, nurses create a comfort care plan to improve comfort by evaluating essential solace. When the patient or family satisfaction increases, they may participate in health-seeking activities more thoroughly, consciously, or subconsciously. In their lives, caregivers incorporate spirituality, self-care, and self-responsibility. This initiative also leads the nurse to a deeper understanding of the interconnections among themselves, others, nature, spirit, and the global community.
In the Comfort Principle, healthcare consumers are viewed as persons, relatives, institutions, and healthcare-related societies. The atmosphere is any factor that can be exploited by a health care professor or a loved person to maximize satisfaction in the patient, family, or institutional environment. The model defines nursing as a process in which patients’ comfort needs will be estimated and suitable nursing care plans created and enforced. Also, it defines patient consolation after treatment plans have been implemented (Aksoy Derya & Pasinlioğlu, 2017). Other than carefully considering the comfort requirements, nursing involves the conception of solace steps to satisfy these needs. Evaluation can be objective, for example, to observe healing wounds, or subjective, to ask the patient if he or she is at ease. The nurse’s job is to determine the patient’s comfort needs and establish a nursing plan to fulfill these needs. With the consolation of a patient shifting, the interventions of the nurse often change. This approach allows nurses to ensure their patients receive adequate treatment and comfort. If one has warmth, physically and psychologically, they may feel better, helping to heal.
Although nursing scholars argue that theory and practical studies are the nursing field’s cornerstones, some nursing practitioners struggle to carry out evidence-based interventions and ensure that these three cornerstones are reciprocal and cyclical. When a nursing practitioner prescribes care for a patient substantiated by scientific studies, she applies evidence-based methods. Often nurses pursue an experimental analysis contrasting the success of a procedure with an untreated control group (Saleh, 2018). Unfortunately, a lack of resources to conduct research studies for the various nursing alternatives can help better the comfort and swift recovery of the ailing patients. Additionally, the unavailability of adequate funds undermines the implementation of the specific recommendations. Also, ignorance about the comfort model’s significance in promoting patient care contributes to the undesirable nursing outcome. For instance, poor relationship between clients and health professionals has seen the caregivers implement approaches that expose the service consumers to either delayed recovery or secondary effects.
The entrusted nursing stakeholders need to invest in research studies about the relationships between the three aspects before making any decision that might harm the patients. For instance, Aksoy Derya and Pasinlioğlu (2017) claim that the professionals should involve all the stakeholders, including the patients and their family members, to suggest the best evidence-based recommendations to boost the professionals’ dream of promoting patients’ swift recoveries and sustainable society.
References
Aksoy Derya, Y., & Pasinlioğlu, T. (2017). The effect of nursing care based on comfort theory on women’s postpartum comfort levels after caesarean sections. International Journal of Nursing Knowledge, 28(3), 138-144.
Saleh, U. S. (2018). Theory guided practice in nursing. Journal of Nursing Research and Practice, 2(1), 18.
